Understanding peroneal tendonitis
What are the peroneal tendons?
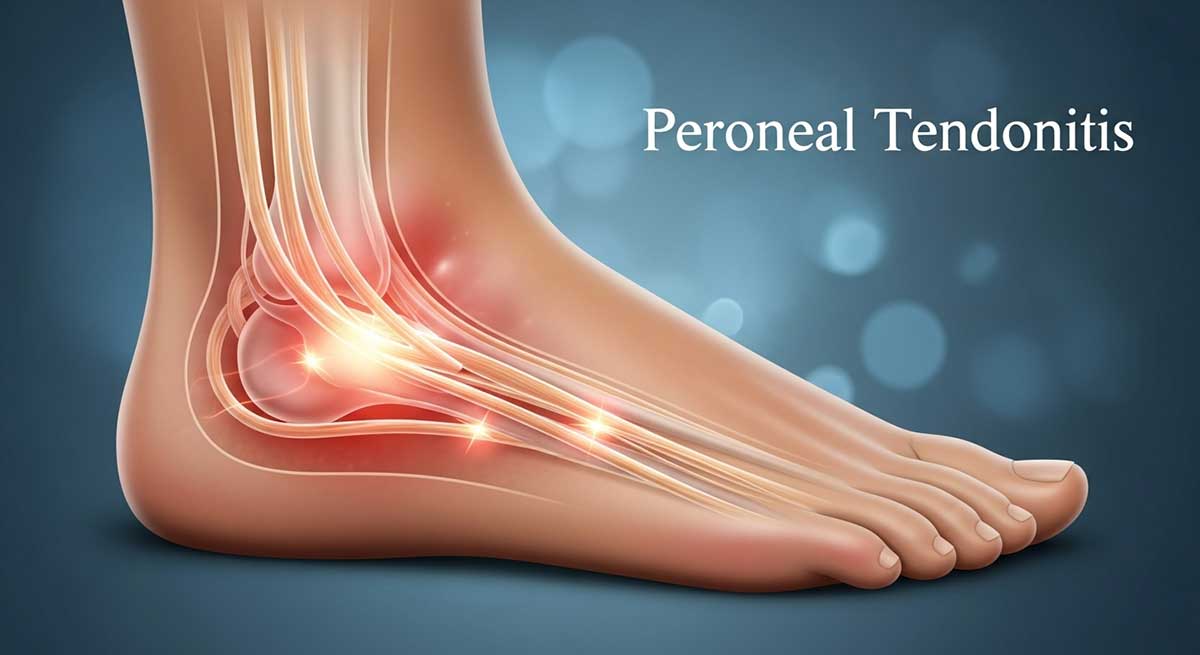
Your peroneal tendons are like strong cables running along the outside of your ankle and foot. Two main tendons make up this system: the peroneus longus and peroneus brevis. These tendons connect muscles in your lower leg to bones in your foot.
The peroneus longus tendon runs behind your outer ankle bone and curves under your foot to attach near your arch. It helps support your arch and turns your foot outward. The peroneus brevis tendon attaches to the outside edge of your foot and provides ankle stability.
Together, these tendons perform three critical functions. They help turn your foot outward (eversion), stabilize your ankle during walking and running, and support your arch to prevent your foot from collapsing inward.
Understanding the biomechanics
When you walk or run, your foot goes through a complex series of movements. Your peroneal tendons work hardest when your foot pushes off the ground and when you land on uneven surfaces. They act like guy-wires on a tent, keeping your ankle stable against forces that try to tip it inward.
Poor foot mechanics can overload these tendons. If your foot rolls inward too much (overpronation) or you have high arches that don’t absorb shock well, your peroneal tendons must work overtime to maintain stability.
What is peroneal tendonitis vs. other conditions?
Peroneal tendonitis involves inflammation and irritation of these tendons. However, chronic cases often develop into tendinopathy, where the tendon structure itself changes. The tendon may thicken, develop scar tissue, or show signs of degeneration.
This differs from peroneal tendon tears, where the tendon actually rips, or peroneal subluxation, where tendons slip out of their normal groove. These conditions require different treatment approaches, which is why proper diagnosis matters.
Research shows that tendinopathy responds better to loading exercises than rest alone. A 2018 study in the British Journal of Sports Medicine found that eccentric loading exercises improved tendon structure and reduced pain in 85% of patients with chronic tendinopathy.
Common symptoms and presentations
Pain typically develops gradually on the outside of your ankle or foot. It often starts as a dull ache after activity but can progress to sharp pain during movement. The pain usually worsens with activities that involve pushing off your foot or walking on uneven ground.
You might notice swelling behind your outer ankle bone or tenderness when you press on the tendons. Some people describe a feeling of ankle instability or weakness, especially when walking on uneven surfaces.
Morning stiffness is common – your ankle may feel tight and sore when you first get out of bed. This usually improves after a few minutes of movement but returns after periods of rest.
What causes peroneal tendonitis?
Understanding the root cause helps prevent future problems and guides your treatment approach.
Overuse and training errors
account for most cases. Runners who suddenly increase their mileage, athletes who intensify training without proper progression, or weekend warriors who go from sedentary to very active face the highest risk. The 10% rule applies here – don’t increase your training load by more than 10% per week.
Biomechanical factors
play a huge role. High arches (cavus feet) create more stress on peroneal tendons because they don’t absorb shock well. Conversely, flat feet can cause different stresses. Previous ankle sprains often leave residual instability that forces peroneal tendons to work harder.
Footwear issues
contribute more than most people realize. Worn-out shoes lose their ability to control foot motion. Shoes that don’t match your foot type or activity can alter your mechanics. Running shoes should be replaced every 300-500 miles, depending on your weight and running style.
Environmental factors
matter too. Running on sloped surfaces forces one foot to work harder than the other. Beach running in soft sand increases the workload on stabilizing muscles. Sudden changes in training surface (from treadmill to trails) can trigger problems.
Muscle imbalances
throughout your body affect your feet. Weak glutes allow your knee to collapse inward, changing how your foot contacts the ground. Tight calf muscles can force your foot into positions that stress the peroneal tendons. Core weakness affects your overall stability and movement patterns.
Why exercise-based treatment works
Exercise therapy addresses the root causes of peroneal tendonitis rather than just masking symptoms. Controlled loading stimulates tendon healing and remodeling. A 2019 systematic review found that exercise therapy was more effective than passive treatments for chronic tendinopathy.
Strengthening exercises build resilience in your peroneal tendons and supporting muscles. This reduces the relative stress on injured tissues and helps prevent re-injury. Balance training improves your proprioception – your body’s ability to sense joint position and movement.
Range of motion exercises prevent the stiffness and adhesions that can develop during healing. Functional exercises prepare your ankle for real-world demands, making your return to activity safer and more successful.
Quick summary: best exercises for peroneal tendonitis
If you’re dealing with peroneal tendonitis, start with these proven exercises:
- Gentle ankle circles – 10 each direction, 3 times daily
- Resistance band eversion – 2 sets of 10-15 reps
- Single-leg balance – Hold for 30 seconds each foot
- Eccentric heel drops – 2 sets of 10 slow repetitions
- Calf stretches – Hold 30 seconds, repeat 3 times
Recovery typically takes 6-12 weeks with consistent exercise. See a healthcare provider if pain persists beyond 2 weeks or worsens with activity.
Quick start guide: take action today
Step 1: assess your pain level
Use this scale to guide your decisions:
- 0-2/10: Mild discomfort – Start Phase 1 exercises
- 3-4/10: Noticeable pain – Begin with gentle range of motion only
- 5-6/10: Moderate pain – Rest and ice, try gentle stretches
- 7-10/10: Severe pain – Seek immediate medical attention
Step 2: start these 3 essential exercises now
- Ankle Alphabet: Trace letters A-Z with your foot, 2 times
- Wall Push Exercise: Press outside of foot against wall, hold 5 seconds, repeat 10 times
- Towel Calf Stretch: Sit and pull toes toward you with towel, hold 20 seconds
Step 3: know when to get help
Contact a healthcare provider immediately if you experience:
- Inability to bear weight on your foot
- Numbness or tingling in your foot
- Severe swelling that doesn’t improve with rest and ice
- Pain that wakes you up at night
Before you start: important considerations
Medical clearance and professional guidance
Some situations require professional evaluation before starting exercises. Schedule an appointment with a healthcare provider if you experience:
- Severe pain that prevents normal walking
- Numbness, tingling, or loss of sensation
- Significant swelling that doesn’t improve with rest and elevation
- History of ankle fractures or previous tendon injuries
- Diabetes or circulation problems
- Pain that has persisted for more than 3 weeks without improvement
A physical therapist can assess your movement patterns, identify contributing factors, and ensure you’re performing exercises correctly. They can also determine if you need additional interventions like manual therapy or temporary bracing.
Understanding pain vs. discomfort
Learning to distinguish between normal exercise discomfort and harmful pain is crucial for safe recovery.
Normal exercise sensations:
- Mild muscle fatigue during or after exercises
- Slight stiffness the morning after exercise that improves with movement
- A gentle stretching sensation during flexibility exercises
- Mild muscle soreness 24-48 hours after exercise (delayed onset muscle soreness)
Warning signs to stop:
- Sharp, shooting pain during exercise
- Pain that gets progressively worse during exercise
- Pain that significantly increases the next day
- Swelling that worsens after exercise
- Any new numbness or tingling
Essential equipment and alternatives
You don’t need expensive equipment for effective rehabilitation. Here’s what works best and budget-friendly alternatives:
| Preferred Equipment | Alternative Options | Cost |
|---|---|---|
| Resistance Band | Towel, Belt, Partner resistance | $5-15 vs Free |
| Foam Roller | Tennis ball, Rolling pin, Water bottle | $15-30 vs $2-5 |
| Balance Board | Pillow, Folded towel, Couch cushion | $20-40 vs Free |
| Step Platform | Sturdy book, Curb, Bottom stair | $25-50 vs Free |
| Exercise Mat | Thick towel, Carpet | $10-25 vs Free |
Pre-exercise assessment
Before starting any exercise program, complete this self-assessment:
Current Pain Level (0-10 scale):
- At rest: ___
- With walking: ___
- With stairs: ___
- With standing on toes: ___
Functional Limitations:
- Can you walk without limping? Yes/No
- Can you stand on your toes without pain? Yes/No
- Can you balance on one foot for 10 seconds? Yes/No
- Do you have morning stiffness lasting more than 30 minutes? Yes/No
Use your answers to determine your starting phase. If you answered “No” to more than two functional questions or have pain scores above 6/10, start with Phase 1 exercises only.
Phase 1: gentle mobilization and pain reduction (weeks 1-2)
This phase focuses on reducing pain and inflammation while maintaining mobility. Your goals are to decrease irritation, promote blood flow, and prevent stiffness.
Pain management strategies
RICE Protocol remains effective for acute symptoms:
- Rest: Avoid activities that worsen pain, but don’t completely stop moving
- Ice: Apply for 15-20 minutes every 2-3 hours during the first 48-72 hours
- Compression: Use an elastic bandage or ankle sleeve for support
- Elevation: Raise your foot above heart level when resting
Activity modification guidelines:
- Reduce walking distance by 50% initially
- Avoid uneven surfaces, hills, and stairs when possible
- Choose supportive shoes for all activities
- Take breaks every 30 minutes if you must stand for long periods
Phase 1 exercise program
Perform these exercises 2-3 times daily. Each session should take 10-15 minutes.
Gentle range of motion exercises
Ankle alphabet
- Starting Position: Sit in a chair with your affected leg extended
- Movement: Use your foot to trace letters A through Z in the air
- Progression: Start with your name, advance to full alphabet
- Key Points: Keep movements slow and controlled, stop if pain increases
Ankle circles
- Starting Position: Sit comfortably with leg extended or elevated
- Movement: Slowly rotate your foot in circles, 10 clockwise, 10 counterclockwise
- Progression: Increase to 15 circles each direction
- Key Points: Move only your ankle, keep your leg still
Gentle towel stretch
- Starting Position: Sit with your affected leg straight in front of you
- Movement: Loop a towel around your foot and gently pull your toes toward you
- Hold: 15-20 seconds, repeat 3 times
- Progression: Increase hold time to 30 seconds
- Key Points: Should feel a gentle stretch in your calf, not pain
Isometric strengthening
Isometric ankle eversion
- Starting Position: Sit in a chair next to a wall with your affected foot against the wall
- Movement: Press the outside of your foot against the wall without moving your ankle
- Hold: 5 seconds, repeat 10 times
- Progression: Increase hold time to 10 seconds
- Key Points: You should feel muscle activation but no joint movement
Isometric ankle inversion
- Starting Position: Sit with the inside of your foot against a wall or table leg
- Movement: Press inward against the immovable object
- Hold: 5 seconds, repeat 10 times
- Progression: Increase hold time to 10 seconds
- Key Points: This balances the eversion strengthening
Isometric plantarflexion
- Starting Position: Sit with your foot flat on the floor
- Movement: Press your foot down into the floor without lifting your heel
- Hold: 5 seconds, repeat 10 times
- Progression: Increase hold time and repetitions
- Key Points: Think about pushing through your whole foot, not just your toes
Gentle soft tissue care
Self-massage techniques
- Use your hands to gently massage your calf muscles with long, smooth strokes
- Apply gentle pressure with your thumb along the outside of your leg (avoid direct pressure on very tender areas)
- Spend 2-3 minutes per session
- Stop if massage increases your symptoms
Foam rolling (if available)
- Roll your calf muscle gently for 30-60 seconds
- Avoid rolling directly over the peroneal tendons if they’re very tender
- Focus on the larger muscle groups that support ankle function
Phase 1 exercise schedule
| Day | Morning | Afternoon | Evening |
|---|---|---|---|
| Daily | Range of motion exercises (5 min) | Isometric exercises (5 min) | Gentle stretching (5 min) |
Progression criteria for phase 2
You’re ready to advance when you can:
- Walk for 20 minutes without increasing pain
- Complete all Phase 1 exercises without discomfort
- Have morning stiffness lasting less than 15 minutes
- Rate your pain at 3/10 or less during daily activities
Phase 2: Building strength and endurance (weeks 3-8)
This phase gradually loads your tendons and builds strength in supporting muscles. You’ll add resistance exercises and begin addressing muscle imbalances throughout your body.
Phase 2 goals and expectations
Your tendons are ready for more challenge. This phase typically lasts 4-6 weeks, though some people need longer. You should notice gradual improvements in strength, pain levels, and confidence with movement.
Don’t expect linear progress. Some days will feel better than others. This is normal and doesn’t mean you’re not healing.
Comprehensive stretching program
Hold each stretch for 30 seconds and repeat 2-3 times. Perform stretching routine twice daily.
Standing calf stretch (gastrocnemius)
- Starting Position: Stand arm’s length from a wall, hands flat against it
- Movement: Step your affected leg back 2-3 feet, keep heel down, lean forward
- Key Points: Keep your back leg straight, heel firmly planted
- Progression: Hold longer, step further back
Standing soleus stretch
- Starting Position: Same as above but closer to wall
- Movement: Bend your back knee while keeping heel down
- Key Points: This targets deeper calf muscles
- Progression: Increase knee bend, hold longer
Peroneal stretch
- Starting Position: Sit with leg extended
- Movement: Use a towel to gently pull your foot inward and upward
- Key Points: Should feel stretch along outside of lower leg
- Progression: Only progress if completely comfortable
Plantar fascia stretch
- Starting Position: Sit and cross affected ankle over opposite knee
- Movement: Pull your toes back toward your shin
- Key Points: Helps address foot mechanics
- Progression: Hold longer, add gentle massage
Progressive strengthening program
Start with light resistance and focus on perfect form. Aim for 2-3 sets of 10-15 repetitions.
Resistance band exercises
Resisted ankle eversion
- Starting Position: Sit with leg extended, band around foot, secured to table leg
- Movement: Turn foot outward against resistance, hold 2 seconds, return slowly
- Sets/Reps: 2 sets of 10, progress to 3 sets of 15
- Progression: Use stronger band, slower movements, single-leg stance
- Key Points: Control the return movement – don’t let band snap back
Resisted ankle inversion
- Starting Position: Band secured on opposite side
- Movement: Turn foot inward against resistance
- Sets/Reps: 2 sets of 10, progress to 3 sets of 15
- Key Points: Maintain muscle balance around ankle
Resisted dorsiflexion
- Starting Position: Band secured in front of you
- Movement: Pull toes toward shin against resistance
- Sets/Reps: 2 sets of 10-15
- Progression: Stronger band, single-leg stance
- Key Points: Strengthens muscles that balance calf muscles
Resisted plantarflexion
- Starting Position: Band around foot, other end held in hands
- Movement: Point foot downward against resistance
- Sets/Reps: 2 sets of 10-15
- Key Points: Don’t just use toes – engage whole foot
Weight-bearing exercises
Double-leg heel raises
- Starting Position: Stand with feet hip-width apart, hands on wall for balance
- Movement: Rise up onto toes, hold 2 seconds, lower slowly
- Sets/Reps: 2 sets of 10, progress to 3 sets of 20
- Progression: Single leg, add weight, off step for greater range
- Key Points: Equal weight on both feet, control the lowering phase
Toe raises
- Starting Position: Stand with back against wall
- Movement: Lift toes while keeping heels down
- Sets/Reps: 2 sets of 15
- Progression: Single leg, hold longer
- Key Points: Balances calf strengthening
Short foot exercise
- Starting Position: Sit with feet flat on floor
- Movement: Try to shorten your foot by pulling toes toward heel without curling them
- Hold: 5 seconds, repeat 10 times
- Progression: Perform standing, add resistance
- Key Points: Activates small muscles that support arch
Eccentric loading program
Eccentric exercises are crucial for tendon healing. They involve lengthening muscles under tension.
Eccentric heel drops
- Starting Position: Stand on a step with balls of feet on edge, heels hanging off
- Movement: Rise up on both feet, then slowly lower on affected leg only (3-5 seconds)
- Sets/Reps: 2 sets of 10, progress to 3 sets of 15
- Progression: Add weight, increase lowering time
- Key Points: The slow lowering is most important part
Eccentric resisted eversion
- Starting Position: Foot turned outward against band resistance
- Movement: Slowly return to center position against band resistance
- Sets/Reps: 2 sets of 10
- Key Points: Focus on controlling the return movement
Phase 2 exercise schedule
| Day | Duration | Focus |
|---|---|---|
| Monday | 25-30 min | Full strengthening routine |
| Tuesday | 15 min | Stretching and range of motion |
| Wednesday | 25-30 min | Full strengthening routine |
| Thursday | 15 min | Stretching and eccentric exercises |
| Friday | 25-30 min | Full strengthening routine |
| Weekend | 10-15 min | Gentle stretching and self-massage |
Troubleshooting common phase 2 problems
“My pain is getting worse”
- Reduce exercise intensity by 25%
- Focus on perfect form over resistance
- Ensure you’re not doing too much too soon
- Consider seeing a healthcare provider if pain persists
“I can’t feel the exercises working”
- Check your form – poor technique reduces effectiveness
- You might need more resistance or repetitions
- Focus on the quality of movement, not just quantity
- Some exercises work stabilizing muscles you can’t easily feel
“I don’t have time for the full routine”
- Prioritize eccentric exercises and balance training
- Break routine into smaller sessions throughout the day
- Focus on 3-4 key exercises done well rather than rushing through everything
Progression criteria for phase 3
You’re ready to advance when you can:
- Complete all Phase 2 exercises without pain
- Perform 15 single-leg heel raises
- Balance on one foot for 30 seconds with eyes closed
- Walk/hike for 45 minutes without symptoms
- Have confidence in your ankle stability
Phase 3: Functional and dynamic training (weeks 9-16)
This phase prepares you for return to full activity. You’ll work on balance, coordination, power, and sport-specific movements.
Phase 3 goals and principles
Your goals shift from basic strength to functional performance. You’ll challenge your ankle stability system with dynamic movements and prepare for the demands of your specific activities.
This phase requires patience. While you may feel much better, your tissues are still adapting. Rushing back to full activity is the most common cause of re-injury.
Advanced balance and proprioception training
Balance training is crucial for preventing re-injury. Your proprioceptive system needs retraining after injury.
Progressive single-leg stance
- Level 1: 30 seconds, eyes open, firm surface
- Level 2: 30 seconds, eyes closed, firm surface
- Level 3: 30 seconds, eyes open, soft surface (pillow)
- Level 4: 30 seconds, eyes closed, soft surface
- Level 5: Add head movements or arm reaches
- Progression: Master each level before advancing
Balance and reach series
- Starting Position: Stand on affected leg
- Movement: Reach forward, backward, and to each side with free leg
- Sets/Reps: 10 reaches each direction
- Progression: Increase reach distance, add unstable surface
- Key Points: Maintain balance throughout movement
Dynamic balance challenges
- Exercise 1: Walk heel-to-toe in straight line (10 steps)
- Exercise 2: Stand on one foot while playing catch
- Exercise 3: Balance while brushing teeth or talking on phone
- Progression: Close eyes, unstable surface, add distractions
Kinetic chain strengthening
Your whole body affects ankle function. These exercises address the complete movement chain.
Proper squat technique
- Starting Position: Feet hip-width apart, toes slightly outward
- Movement: Sit back like sitting in chair, knees track over toes
- Sets/Reps: 2-3 sets of 10-15
- Progression: Add weight, single leg, jump squats
- Key Points: Equal weight on both feet, don’t let knees cave inward
Lateral lunges
- Starting Position: Stand with feet together
- Movement: Step wide to one side, bend that knee, push back to center
- Sets/Reps: 2 sets of 10 each direction
- Progression: Add weight, increase range of motion
- Key Points: Keep chest up, don’t let knee cave inward
Step-up progressions
- Level 1: Step up slowly, step down slowly (6-8 inch step)
- Level 2: Step up quickly, step down slowly
- Level 3: Add knee drive at top
- Level 4: Lateral step-ups
- Sets/Reps: 2 sets of 10 each leg
- Key Points: Control the step-down phase
Hip strengthening series
- Side-lying leg lifts: 2 sets of 15 each side
- Clamshells: 2 sets of 15 each side
- Lateral band walks: 2 sets of 10 steps each direction
- Key Points: Strong glutes prevent knee and ankle collapse
Introduction to plyometric training
Add jumping exercises only when you can perform all previous exercises pain-free. Start very conservatively.
Double-leg hop progressions
- Level 1: Small hops in place (10 reps)
- Level 2: Forward and backward hops (5 each direction)
- Level 3: Side-to-side hops (5 each direction)
- Key Points: Focus on soft landings with bent knees
Single-leg hop progressions
- Level 1: Hop in place on good leg, then affected leg (5 reps each)
- Level 2: Forward hop and stick landing (3 reps)
- Level 3: Lateral hop and stick landing (3 reps)
- Progression: Only advance if completely pain-free
Box jump progressions
- Level 1: 6-8 inch box, focus on landing mechanics
- Level 2: 10-12 inch box
- Level 3: Single-leg box jumps (advanced)
- Key Points: Step down, don’t jump down
Sport-specific training progressions
Tailor your training to your specific activities:
For runners:
- Start with walk-run intervals: 2 minutes walk, 1 minute easy jog
- Progress to continuous easy running
- Add hills and speed work gradually
- Focus on cadence around 170-180 steps per minute
For court sports (basketball, tennis):
- Start with straight-line jogging
- Add gentle cutting movements
- Progress to sport-specific drills
- Practice jump-landing mechanics extensively
For hikers:
- Start on flat, even trails
- Progress to gentle hills
- Add uneven terrain gradually
- Practice downhill walking technique
Phase 3 exercise schedule
| Day | Duration | Focus |
|---|---|---|
| Monday | 35-40 min | Full functional routine |
| Tuesday | 20 min | Balance and proprioception |
| Wednesday | 35-40 min | Full functional routine |
| Thursday | 25 min | Sport-specific training |
| Friday | 35-40 min | Full functional routine |
| Saturday | 30 min | Active recovery (easy walk, gentle stretching) |
| Sunday | Rest or 15 min gentle movement |
Exercise progression and modification system
Systematic progression guidelines
Progressive overload is key to continued improvement. Here’s how to systematically advance your exercises:
| Exercise Component | Beginner | Intermediate | Advanced |
|---|---|---|---|
| Resistance | Body weight, light band | Medium band, light weights | Heavy band, moderate weights |
| Repetitions | 8-10 | 12-15 | 15-20 |
| Sets | 1-2 | 2-3 | 3-4 |
| Hold Time | 2-3 seconds | 3-5 seconds | 5+ seconds |
| Balance Challenge | Eyes open, firm surface | Eyes closed, firm surface | Eyes closed, unstable surface |
| Speed | Slow, controlled | Moderate pace | Variable speeds |
Exercise modification matrix
| Exercise | Easier Version | Standard Version | Harder Version |
|---|---|---|---|
| Heel Raises | Both feet, hands on wall | Both feet, no support | Single leg, add weight |
| Eversion | Seated, light band | Standing, medium band | Single leg stance, heavy band |
| Balance | Both feet, eyes open | Single leg, eyes open | Single leg, eyes closed, unstable |
| Squats | Chair-assisted | Body weight | Add weight, single leg |
| Lunges | Stationary, hand support | Full range, no support | Add weight, jump lunges |
The 24-hour assessment rule
Monitor your response to exercise using this systematic approach:
Immediately after exercise:
- Mild muscle fatigue is normal
- Sharp pain is not normal
- Increased swelling is concerning
2-4 hours after exercise:
- Some muscle soreness is normal
- Increased tendon pain suggests too much intensity
- New symptoms need attention
Next morning:
- Mild stiffness that improves with movement is normal
- Increased pain or stiffness suggests overload
- Inability to bear weight requires medical attention
Regression strategies when needed
Sometimes you need to step back. This isn’t failure – it’s smart management.
When to regress:
- Pain increases during or after exercise
- New symptoms develop
- You can’t maintain proper form
- You’re not recovering between sessions
How to regress:
- Reduce resistance by 25-50%
- Decrease repetitions by 20-30%
- Increase rest time between sets
- Return to previous phase exercises
- Focus on perfect form over challenge
Sample exercise programs
Beginner weekly schedule
Start with 3 days per week, with at least one rest day between sessions. A sample week might look like:
- Monday: Phase 1 exercises (15 minutes)
- Wednesday: Phase 1 exercises (15 minutes)
- Friday: Phase 1 exercises (15 minutes)
Intermediate weekly schedule
As you progress, you can exercise more frequently:
- Monday: Phase 2 exercises (20-25 minutes)
- Tuesday: Gentle stretching and range of motion (10 minutes)
- Thursday: Phase 2 exercises (20-25 minutes)
- Friday: Balance and proprioception focus (15 minutes)
- Sunday: Gentle stretching and range of motion (10 minutes)
Advanced weekly schedule
When you’re ready for Phase 3 exercises:
- Monday: Full strengthening routine (30 minutes)
- Tuesday: Balance and functional exercises (20 minutes)
- Wednesday: Maintenance exercises (15 minutes)
- Thursday: Full strengthening routine (30 minutes)
- Friday: Sports-specific exercises (25 minutes)
- Saturday: Active recovery – gentle walking or swimming
- Sunday: Rest or very light stretching
Integrating exercises into your day
Make exercises part of your routine. Do calf stretches while brushing your teeth. Practice balance exercises while waiting for coffee to brew. Perform toe raises while watching TV.
Comprehensive exercise programs by phase
Phase 1 complete program (weeks 1-2)
Daily routine (15 minutes, 2-3 times per day):
Morning (5 minutes):
- Ankle alphabet (2 minutes)
- Gentle ankle circles (1 minute)
- Towel calf stretch (2 minutes)
Midday (5 minutes):
- Isometric eversion (2 minutes)
- Isometric inversion (2 minutes)
- Gentle self-massage (1 minute)
Evening (5 minutes):
- Repeat morning routine
- Add ice if needed (15-20 minutes)
Phase 2 complete program (weeks 3-8)
Monday/Wednesday/Friday – strength focus (25-30 minutes):
Warm-up (5 minutes):
- Ankle circles and alphabet
- Gentle calf stretches
Strengthening (15 minutes):
- Resisted eversion: 2 sets × 12 reps
- Resisted inversion: 2 sets × 12 reps
- Resisted dorsiflexion: 2 sets × 12 reps
- Heel raises: 2 sets × 15 reps
- Toe raises: 2 sets × 15 reps
- Short foot exercise: 2 sets × 10 reps
Eccentric focus (5 minutes):
- Eccentric heel drops: 2 sets × 10 reps
- Eccentric eversion: 2 sets × 10 reps
Cool-down (5 minutes):
- Hold all stretches for 30 seconds each
Tuesday/Thursday – flexibility and recovery (15 minutes):
- Complete stretching routine
- Gentle range of motion
- Self-massage techniques
Phase 3 complete program (weeks 9-16)
Monday/Wednesday/Friday – full functional (35-40 minutes):
Dynamic warm-up (8 minutes):
- Light walking or marching
- Ankle circles and movements
- Gentle bodyweight squats
Strength circuit (20 minutes):
- Squats: 3 sets × 12 reps
- Single-leg heel raises: 3 sets × 10 reps each
- Lateral lunges: 2 sets × 10 each direction
- Resisted eversion (standing): 2 sets × 15 reps
- Step-ups: 2 sets × 10 each leg
- Hip strengthening series: 2 sets × 15 each
Balance and proprioception (7 minutes):
- Single-leg stance progressions: 3 × 30 seconds each
- Balance and reach: 2 sets × 8 each direction
- Dynamic balance challenges: 5 minutes
Cool-down (5 minutes):
- Complete stretching routine
Tuesday/Thursday – sport-specific (25 minutes):
- Dynamic warm-up (5 minutes)
- Sport-specific drills (15 minutes)
- Cool-down stretching (5 minutes)
Preventing peroneal tendonitis recurrence
Continued maintenance exercises
Don’t stop exercising once your pain goes away. Continue with a maintenance program 2-3 times per week. Focus on key exercises like heel raises, balance work, and peroneal strengthening.
A simple maintenance routine might include:
- 10 single-leg heel raises each side
- 30-second single-leg stance each side
- 15 resisted eversion exercises each side
- Calf stretches
Proper footwear choices
Invest in good shoes that support your feet. Replace running shoes every 300-500 miles or when the tread wears unevenly. For daily wear, choose shoes with good arch support and cushioning.
Consider your activity when choosing shoes. Tennis shoes work well for lateral movements, while running shoes are designed for forward motion. Using the right shoe for your activity reduces injury risk.
Gradual training progression
The 10% rule provides a good guideline for increasing activity. Don’t increase your training volume by more than 10% per week. This applies to running mileage, workout intensity, or any new activity.
Your body needs time to adapt to new demands. Rushing back to full activity often leads to re-injury. Be patient with your progression.
Warm-ups and cool-downs
Always warm up before activity and cool down afterward. A good warm-up includes 5-10 minutes of gentle movement that gradually increases your heart rate and prepares your muscles for more intense activity.
Cool-downs help your body recover and can prevent stiffness. Include gentle stretching and a gradual return to rest.
Addressing biomechanical issues
If you have flat feet, high arches, or other structural issues, you might benefit from arch supports or custom orthotics. A podiatrist or physical therapist can assess whether these would help you.
Don’t ignore recurring problems. If you keep getting peroneal tendonitis despite following a good exercise program, there might be an underlying biomechanical issue that needs professional attention.
Listening to your body
Early intervention prevents small problems from becoming big ones. If you notice familiar symptoms returning, don’t ignore them. Return to your rehabilitation exercises and modify your activities until symptoms resolve.
Beyond exercises: complementary strategies
Acute care strategies
For sudden flare-ups, remember RICE: Rest, Ice, Compression, and Elevation. Ice for 15-20 minutes several times per day can help reduce inflammation. Compression with an elastic bandage provides support, and elevation helps reduce swelling.
These strategies work best in the first 48-72 hours after symptom onset. After that, focus on gentle movement and exercises.
Professional treatment options
Physical therapists can provide manual therapy techniques that complement your exercise program. They might use joint mobilization, soft tissue massage, or other techniques to improve your recovery.
Some people benefit from temporary taping or bracing, especially during the return to sports. These should be used under professional guidance and as part of a comprehensive treatment plan.
Nutrition for tendon health
While no specific foods cure tendonitis, good nutrition supports healing. Stay well-hydrated and eat a balanced diet rich in anti-inflammatory foods like fish, leafy greens, and berries.
Adequate protein intake helps with tissue repair. Vitamin C supports collagen production, which is important for tendon health.
When to progress and return to full activity
Milestones for progression
You’re ready to progress to the next phase when you can complete your current exercises without pain. You should be able to walk without discomfort and perform daily activities normally.
Specific milestones include:
- No pain during normal walking
- Ability to rise up on your toes without pain
- Completion of all phase exercises without symptoms
- No morning stiffness or pain
Guidelines for gradual return to sport
Returning to demanding activities requires patience. Start with low-intensity, short-duration activities and gradually increase both intensity and duration.
For runners, this might mean starting with walk-run intervals before returning to continuous running. For court sports, begin with straight-line activities before adding cutting and jumping movements.
Managing setbacks
Setbacks are normal during recovery. If symptoms return, don’t panic. Return to easier exercises and reduce your activity level temporarily. Most setbacks resolve quickly with appropriate management.
If setbacks are frequent or severe, consider consulting a healthcare provider. There might be factors you haven’t addressed that are contributing to your problems.
Conclusion
Recovery from peroneal tendonitis requires patience, consistency, and the right approach. The exercises in this guide address not just your symptoms, but the underlying factors that contributed to your problem.
Start with gentle exercises and progress gradually. Listen to your body and adjust your program as needed. Remember that everyone heals at their own pace – don’t compare your recovery to others.
The key principles for success are:
- Consistency with your exercise program
- Gradual progression without rushing
- Addressing the whole kinetic chain, not just your ankle
- Proper warm-ups and cool-downs
- Appropriate footwear and training practices
With the right approach, most people can successfully recover from peroneal tendonitis and return to their favorite activities. The exercises and strategies in this guide give you the tools you need to take control of your recovery and prevent future problems.
Your peroneal tendons are resilient structures that respond well to appropriate exercise. By following this progressive program and maintaining good habits, you can get back to pain-free activity and keep your ankles healthy for years to come.
FAQs
How long does it take to recover with exercises?
Recovery time varies greatly depending on the severity of your condition and how long you’ve had symptoms. Acute cases might improve in 2-4 weeks, while chronic problems can take 3-6 months or longer.
Consistency with your exercise program is more important than the specific timeline. Stick with your program even if progress seems slow.
Can I run with peroneal tendonitis?
Running with active peroneal tendonitis often makes symptoms worse. It’s better to take time off running and focus on rehabilitation exercises. You can maintain fitness with activities like swimming or cycling that don’t stress your peroneal tendons.
Once your symptoms improve, you can gradually return to running following the guidelines above.
Are there any exercises I should avoid?
Avoid exercises that cause sharp pain or significantly increase your symptoms. High-impact activities like jumping or running on uneven surfaces often need to be avoided initially.
Exercises that force your ankle into extreme positions might also be problematic. Stick with pain-free ranges of motion, especially early in your recovery.
Should the exercises be painful?
Exercises should not cause sharp pain or significantly increase your symptoms. Some muscle fatigue or mild discomfort is normal, especially as you build strength.
Use the 24-hour rule: if your symptoms are worse the day after exercising, you did too much. Reduce the intensity or duration of your program.
What if I don’t have resistance bands?
You can still do effective exercises without equipment. Use a towel for resistance, perform exercises against a wall, or use your own body weight for resistance.
Isometric exercises work well without equipment. Balance exercises only require a stable surface. While resistance bands are helpful, they’re not absolutely necessary.


