Your bones aren’t static. They’re alive, constantly breaking down and rebuilding themselves in a process that never stops. Yet most people don’t think about their skeleton until something breaks.
Osteoporosis steals bone density so quietly that it’s earned the nickname “the silent thief.” By the time you feel pain or suffer a fracture, you’ve already lost substantial bone mass. And while exercise and a solid diet form your first line of defense, many people need extra support.
Walk into any pharmacy, and you’ll face a wall of bone-health supplements. Calcium pills in every dose imaginable. Vitamin D bottles with wildly different strengths. Collagen powders promising youth. Which ones actually work?
How to Know If You Need Supplements
Before you buy anything, ask yourself these questions. Your answers will tell you if supplements make sense for your situation.
If you checked two or more boxes, talk with your doctor about a DEXA scan. This quick, painless test measures your bone mineral density and shows whether you have osteopenia (low bone mass) or osteoporosis.
Blood tests worth requesting:
Your doctor can check vitamin D levels (aim for 30-50 ng/mL), calcium, magnesium, and parathyroid hormone. These tests reveal deficiencies that diet changes or targeted supplements can fix. Guessing wastes money. Testing gives you answers.
Men under 70 and pre-menopausal women without risk factors can usually maintain bone health through diet and exercise alone. But if you’re deficient in key nutrients, you’ll need supplementation regardless of age.
Bone Health Risk Assessment
Answer these questions to understand your bone health risk
Daily Nutrient Targets: What You Actually Need
Here’s what you’re aiming for based on your age and sex:
| Nutrient | Women 19-50 | Women 51+ | Men 19-70 | Men 71+ |
|---|---|---|---|---|
| Calcium | 1,000 mg | 1,200 mg | 1,000 mg | 1,200 mg |
| Vitamin D | 600 IU (minimum) | 800 IU (minimum) | 600 IU (minimum) | 800 IU (minimum) |
| Protein | 0.8 g/kg bodyweight | 1.0-1.2 g/kg | 0.8 g/kg | 1.0-1.2 g/kg |
| Magnesium | 310-320 mg | 320 mg | 400-420 mg | 420 mg |
| Vitamin K | 90 mcg | 90 mcg | 120 mcg | 120 mcg |
These are minimums. Many bone health experts suggest higher vitamin D levels (2,000-4,000 IU daily) when deficiency exists, but blood testing should guide your specific dose.
1: Calcium (But Not How You Think)
Calcium gets all the attention. And for good reason—it’s the main mineral in your bones. Studies consistently show that getting enough calcium helps reduce fracture risk in older adults, particularly when combined with vitamin D.
A comprehensive review analyzing multiple randomized controlled trials found that combined calcium and vitamin D supplementation reduces fracture risk, especially hip and other major fractures, in older adults with insufficient intake or low baseline vitamin D levels. The benefit appears strongest in those over 70 and in people who were deficient to begin with.
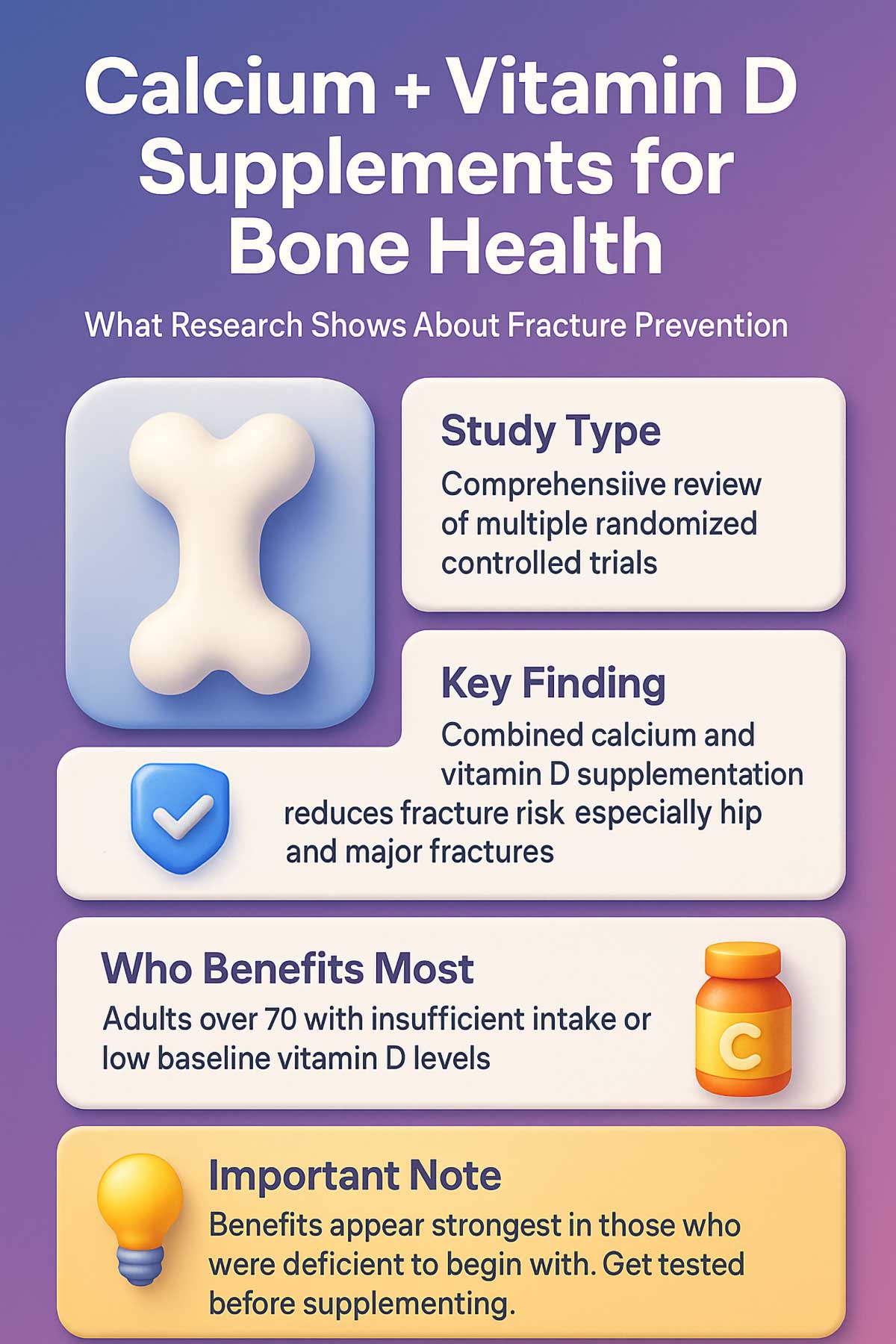
But here’s the catch: more isn’t always better.
Your body needs about 1,000 to 1,200 mg of calcium daily, depending on your age and sex. The problem? High-dose calcium supplements have raised concerns about arterial calcification—calcium deposits in your blood vessels instead of your bones. Some research suggests that calcium from pills may increase this risk more than calcium from food.
Dietary calcium from dairy, leafy greens, fortified plant milks, and sardines doesn’t carry the same concerns. Your body processes food-based calcium differently, absorbing it more gradually and safely.
The smart approach: Get as much calcium as you can from food. If you fall short, use a modest supplement to bridge the gap—not to blast past your daily needs. Think calcium management, not calcium overload.
How Much Calcium Are You Really Getting?
Most people overestimate their calcium intake. Here’s what common foods actually provide:
| Food | Serving Size | Calcium Content |
|---|---|---|
| Plain yogurt | 1 cup | 450 mg |
| Cheddar cheese | 1.5 oz | 300 mg |
| Sardines with bones | 3 oz | 325 mg |
| Fortified almond milk | 1 cup | 450 mg |
| Cooked collard greens | 1 cup | 270 mg |
| Tofu (calcium-set) | 1/2 cup | 250-750 mg |
| Chia seeds | 2 tbsp | 180 mg |
| Almonds | 1 oz (23 nuts) | 75 mg |
| White beans | 1 cup cooked | 160 mg |
Track your intake for three days. Add up the calcium from everything you eat. If you consistently fall 300-400 mg short of your target, a small supplement makes sense. If you’re hitting 1,000 mg from food alone, you probably don’t need more.
Calcium Intake Calculator
Track your daily calcium intake and see if you're meeting your needs
Your Profile
Add Foods You Eat
2: Vitamin D3
Imagine trying to open a locked door. You can push all you want, but without the key, you’re not getting through. That’s calcium without vitamin D.
Vitamin D acts as the key that unlocks calcium absorption in your gut. Without adequate levels, your body can’t use the calcium you consume, whether from food or supplements. This is why calcium and vitamin D are often studied together—they’re a package deal.
Research shows that correcting vitamin D deficiency is critical for maintaining bone mineral density and reducing fracture risk. Yet routine mega-dosing has come under scrutiny. Too much vitamin D can cause problems, including hypercalcemia (too much calcium in your blood).
Studies examining vitamin D supplementation show mixed results when given alone at high doses without addressing actual deficiency. The benefit becomes clear when you’re truly deficient or when vitamin D pairs with adequate calcium intake.
The smart approach: Get your vitamin D levels tested. The ideal blood level typically falls between 30 and 50 ng/mL, though some experts recommend slightly higher targets. Your doctor can help you find your specific dose based on your current levels, typically ranging from 1,000 to 4,000 IU daily.
Don’t guess. Test.
Most adults living in northern climates or spending significant time indoors have some degree of vitamin D insufficiency. Your skin makes vitamin D from sun exposure, but sunscreen, clothing, darker skin tones, and winter months all reduce production.
Very few foods contain meaningful amounts of vitamin D naturally. Fatty fish like salmon and sardines provide some. Fortified milk and plant milks offer about 100 IU per cup. You’d need to drink 10 cups of milk daily to reach even 1,000 IU. That’s why supplementation makes sense for most people.
3: Vitamin K2
This is where most bone-health advice falls short.
Vitamin D helps you absorb calcium. But once calcium enters your bloodstream, where does it go? Ideally, into your bones. But without vitamin K2, calcium can end up in your arteries instead—exactly where you don’t want it.
Vitamin K2, specifically the MK-7 form, activates a protein called osteocalcin. Think of osteocalcin as a construction worker that grabs calcium molecules and cements them into your bone matrix. Without K2, this worker sits idle.
A 2024 systematic review analyzing randomized controlled trials in middle-aged and older adults found that vitamin K2 supplementation increases lumbar spine bone mineral density and improves bone metabolism markers, particularly osteocalcin carboxylation. When combined with calcium and vitamin D, it may reduce fracture risk more effectively than calcium and D alone.
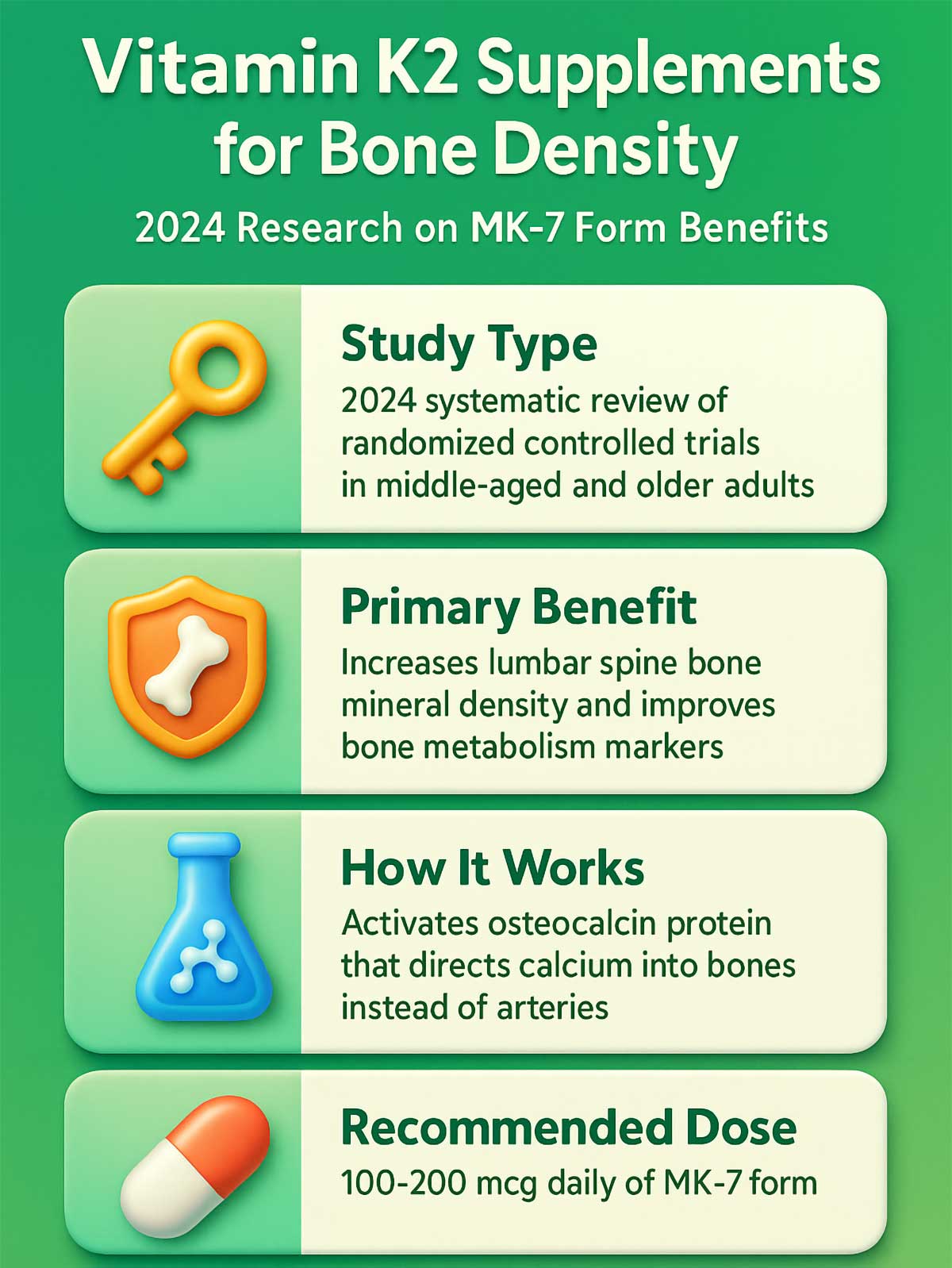
The synergy is simple: D3 absorbs the calcium, K2 directs it to your bones instead of your arteries.
Studies suggest K2 works best at the lumbar spine, with effects building over 6-12 months of consistent supplementation. The biological rationale is strong—vitamin K2 activates proteins that regulate where calcium gets deposited throughout your body.
The smart approach: Look for supplements that pair D3 with K2. Typical doses range from 100 to 200 mcg of K2 (MK-7 form) daily. This combo helps ensure calcium lands where it should.
If you take blood thinners like warfarin, talk with your doctor before adding K2. It can interfere with these medications.
4: Collagen Peptides
Most people think of collagen as a beauty supplement—something for smooth skin and shiny hair. But your bones are actually 90% collagen before they’re mineralized with calcium.
Think of bone structure like reinforced concrete. The collagen provides the steel rebar framework, and minerals like calcium fill in around it. Without strong rebar, the concrete crumbles.
A 2025 meta-analysis examined studies on collagen peptide supplementation in post-menopausal women with osteopenia or osteoporosis. The results showed consistent improvements in bone mineral density at both the spine and femoral neck (hip) compared to control groups. Bone turnover markers also improved, suggesting collagen helps maintain the bone remodeling process.
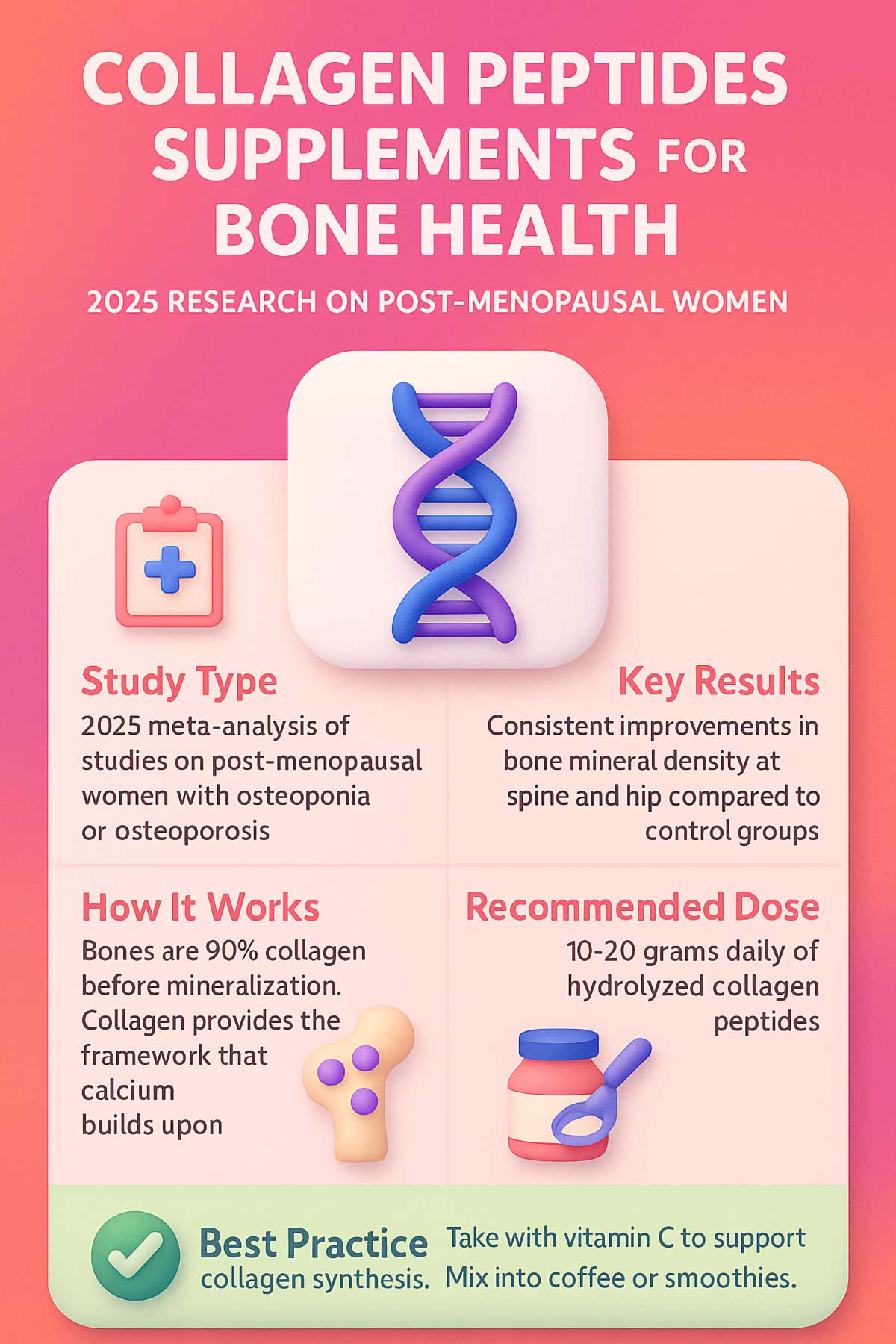
The research focused primarily on specific collagen peptides—hydrolyzed collagen broken down into smaller peptides your body can absorb and use. These peptides appear to stimulate bone-forming cells called osteoblasts while supporting the collagen matrix that gives bones their flexibility and fracture resistance.
The science is still developing, but the evidence is promising—particularly for post-menopausal women who face accelerated bone loss. Collagen supplementation, often combined with calcium and vitamin D in studies, shows benefits beyond what minerals alone provide.
The smart approach: Consider hydrolyzed collagen peptides at 10 to 20 grams daily. Mix it into your morning coffee or smoothie. Choose products that specify “collagen peptides” or “hydrolyzed collagen” for better absorption.
Collagen is tasteless and dissolves easily in hot or cold liquids. Some people notice improvements in joint comfort as a bonus benefit, though bone health benefits take several months to manifest.
5: Magnesium
Here’s something most people miss: vitamin D sits dormant in your body until magnesium activates it. Your liver and kidneys convert vitamin D into its active form—but this conversion requires magnesium as a cofactor.
Low magnesium means low active vitamin D, no matter how much D you swallow. And many people don’t get enough magnesium. Modern diets often fall short, and stress, alcohol, and certain medications deplete it further.
Magnesium also plays direct roles in bone formation and influences the activity of bone cells. Research examining overall bone health consistently points to magnesium as a critical supporting nutrient alongside calcium, vitamin D, and K2. Magnesium deficiency or low intake may impair bone health and increase fracture risk.
More than half of your body’s magnesium lives in your bones, where it contributes to the physical structure and influences calcium metabolism. Studies show that higher magnesium intake correlates with higher bone mineral density across various age groups.
The smart approach: Aim for 300 to 400 mg of magnesium daily. Choose magnesium glycinate or citrate—these forms absorb better than magnesium oxide. Many people take it at night since it can promote relaxation and better sleep.
If your vitamin D levels won’t budge despite supplementation, low magnesium might be the culprit.
Foods rich in magnesium include dark leafy greens, nuts, seeds, beans, and whole grains. But soil depletion and food processing reduce the magnesium content of many foods, making supplementation beneficial for many adults.
6: Protein
For years, people believed high protein intake “leached” calcium from bones. This myth needs to die.
A systematic review analyzing multiple studies found that higher protein intake correlates with higher bone density when calcium intake is adequate. The analysis showed that protein supplementation, particularly when combined with sufficient calcium and vitamin D, supports bone health and reduces bone loss compared with low-protein diets.
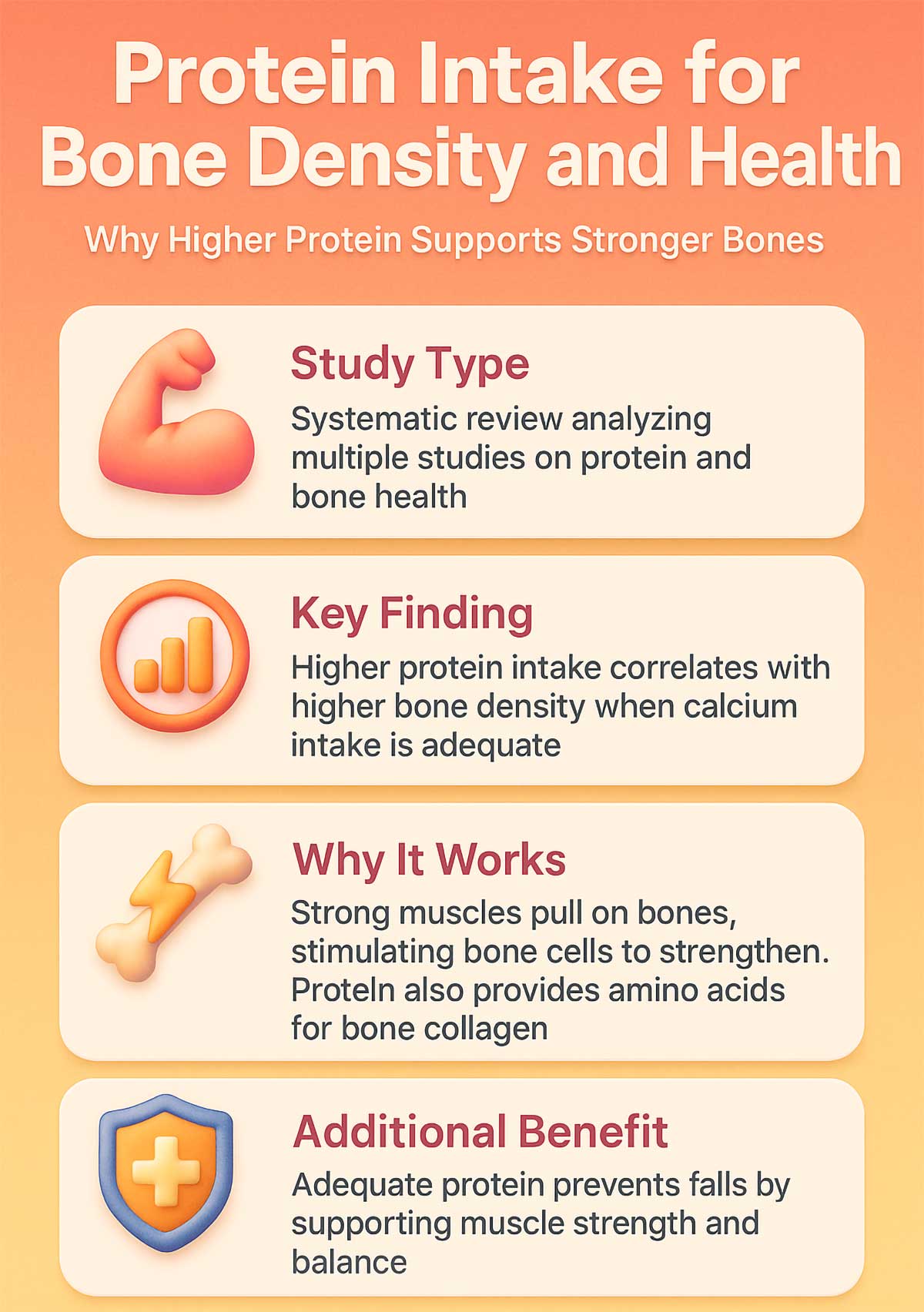
The reason makes mechanical sense. Strong muscles pull on bones during movement, creating tension that stimulates bone cells to strengthen and adapt. This mechanical loading signals your skeleton to maintain or build density. Lose muscle mass, and you lose this bone-strengthening signal.
Plus, adequate protein helps prevent falls—a major cause of fractures in older adults. Protein supports muscle strength, balance, and faster recovery if you do fall. Studies consistently show that older adults with higher protein intake have lower fracture rates, even after adjusting for other factors.
Protein also provides amino acids your body needs to build bone collagen matrix. Your skeleton constantly remodels, and without sufficient protein, you can’t maintain the structural framework.
The smart approach: Aim for about 1.0 to 1.2 grams of protein per kilogram of body weight daily if you’re over 50. For a 150-pound (68 kg) person, that’s roughly 68 to 82 grams. Spread it across meals for better muscle protein synthesis. Don’t fear the protein shake—your bones need it.
Good protein sources include lean meats, fish, eggs, dairy, beans, lentils, tofu, and Greek yogurt. Many of these foods also provide calcium, making them doubly valuable for bone health.
7: Fish Oil and Bone Health
The relationship between omega-3 fatty acids and bone health is more complex than calcium or vitamin D. While omega-3s from fish oil aren’t a primary bone supplement, they play a supporting role in reducing inflammation that can accelerate bone loss.
Studies examining omega-3 supplementation alone show mixed results. Some research suggests that EPA and DHA (the main omega-3s in fish oil) may help preserve bone mineral density, particularly when combined with calcium supplementation. The theory is that omega-3s reduce inflammatory cytokines that stimulate osteoclasts—the cells that break down bone.
A few studies have found that higher omega-3 intake correlates with better bone density in older adults, especially women. But the evidence isn’t as strong or consistent as it is for calcium, vitamin D, or vitamin K2.
The smart approach: If you’re already taking fish oil for heart health or inflammation, you may be getting a modest bone benefit as well. But don’t rely on omega-3s as your primary bone-health strategy. They work best as part of a comprehensive approach that includes calcium, vitamin D, K2, and weight-bearing exercise.
Typical doses studied range from 1,000 to 2,000 mg of combined EPA and DHA daily. Eating fatty fish like salmon, mackerel, or sardines two to three times per week provides omega-3s along with vitamin D and protein—a better overall package for bone health.
8: Glucosamine and Chondroitin
You’ve probably heard of glucosamine and chondroitin for joint health. These supplements support cartilage—the cushioning tissue between bones. But can they help bones themselves?
The research is limited and mixed. Glucosamine and chondroitin primarily target joint cartilage, not bone mineral density. Some animal studies suggest glucosamine might have modest effects on bone metabolism, but human studies haven’t consistently shown bone-building benefits.
That said, there’s an indirect connection worth noting. Healthy joints encourage movement and weight-bearing activity. If glucosamine helps reduce joint pain and keeps you active, that activity benefits your bones. The mechanical loading from walking, dancing, or strength training stimulates bone formation.
The smart approach: If you have osteoarthritis and glucosamine helps you stay active, keep taking it for your joints. But don’t expect it to build bone density directly. Focus on proven bone supplements like calcium, vitamin D, K2, and magnesium instead.
Typical glucosamine doses range from 1,500 mg daily. Chondroitin is often combined at 800 to 1,200 mg. These supplements are generally safe but take several months to show effects on joint symptoms.
9: Blackcurrant Extract and Bone Health
Here’s something new from 2024 research: blackcurrant extract may support bone health through its high anthocyanin content. Anthocyanins are powerful antioxidants that give dark berries their deep purple color.
A 2024 study examined blackcurrant supplementation in post-menopausal women. The results showed improvements in bone turnover markers—specifically, reduced markers of bone breakdown and increased markers of bone formation. The researchers theorized that anthocyanins reduce oxidative stress and inflammation that accelerate bone loss.
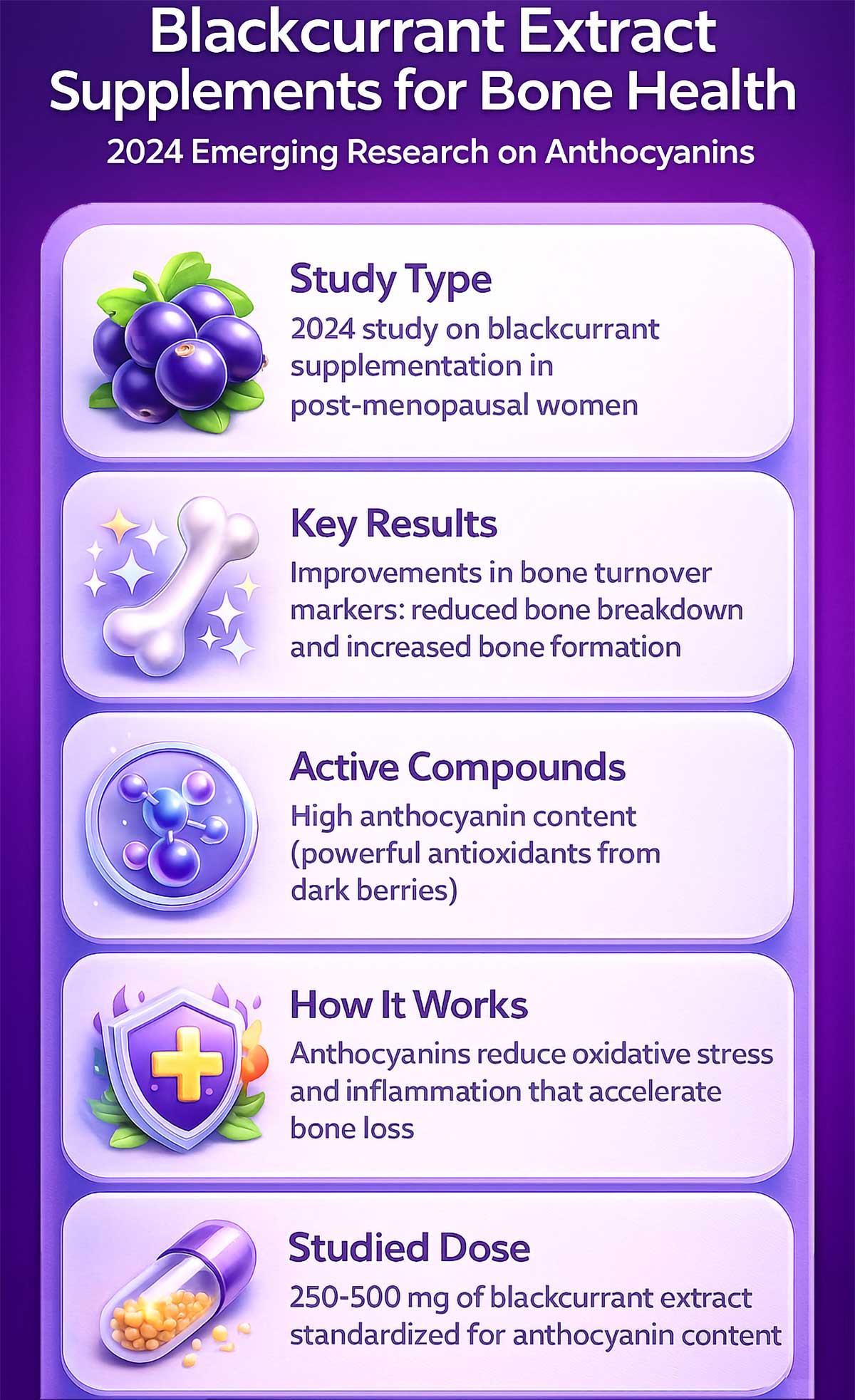
This research is still early. We don’t yet have long-term studies showing whether blackcurrant extract actually increases bone mineral density or reduces fracture risk. But the biological mechanisms make sense, and the preliminary data looks promising.
The smart approach: Consider blackcurrant extract an interesting addition to a comprehensive bone-health program, not a replacement for proven interventions. If you’re post-menopausal and already taking calcium, vitamin D, K2, and magnesium, blackcurrant might offer additional support.
Studies used doses ranging from 250 to 500 mg of blackcurrant extract standardized for anthocyanin content. Look for products that specify anthocyanin concentration. You can also eat fresh or frozen blackcurrants, blueberries, and other dark berries for similar compounds along with vitamin C and fiber.
10: Probiotics and Bone Health
Your gut and your bones talk to each other more than you’d think. Recent research has revealed that gut bacteria influence bone metabolism through several pathways. This emerging field—called the gut-bone axis—suggests that probiotics might support bone health.
Here’s how it works: certain gut bacteria help you absorb calcium and other minerals more efficiently. They also produce short-chain fatty acids that reduce inflammation throughout your body, including in bone tissue. Some bacterial strains may even influence hormone levels that affect bone remodeling.
Studies in animals show clear benefits. Probiotic supplementation increases bone density in mice and rats. Human studies are fewer and smaller, but early results suggest probiotics may help preserve bone mass, particularly in post-menopausal women.
A 2024 review examined several human trials. Some studies found that specific probiotic strains (particularly Lactobacillus and Bifidobacterium species) reduced bone loss markers in older women. Other studies showed no significant effects. The inconsistency likely reflects differences in bacterial strains, doses, and study populations.
The smart approach: Probiotics won’t replace calcium and vitamin D, but they might offer modest additional support—especially if you have digestive issues that impair nutrient absorption. Conditions like celiac disease, Crohn’s disease, and ulcerative colitis damage the gut lining and reduce mineral absorption. Probiotics may help restore gut health and improve nutrient uptake.
Look for multi-strain probiotics with at least 10 billion CFUs (colony-forming units) daily. Lactobacillus reuteri and Lactobacillus rhamnosus are two strains with some bone-health research behind them.
You can also support your gut bacteria through diet. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha provide beneficial bacteria. Prebiotic foods like onions, garlic, leeks, asparagus, and bananas feed the good bacteria already living in your gut.
Timing and Absorption: When to Take What
Taking the right supplements at the wrong time wastes money and reduces effectiveness. Some nutrients compete for absorption. Others work better with food or on an empty stomach.
Here’s what actually matters:
| Supplement | Best Time | Take With | Avoid Taking With | Why |
|---|---|---|---|---|
| Calcium | With meals | Vitamin D | Iron, zinc, thyroid meds (separate by 4 hrs) | Needs stomach acid; blocks absorption of other minerals |
| Vitamin D3 + K2 | Morning with fat | Healthy fats (eggs, avocado, nuts) | Empty stomach | Fat-soluble vitamins need dietary fat |
| Magnesium | Evening | Food | Calcium (separate by 2+ hrs) | Promotes relaxation; competes with calcium for absorption |
| Collagen | Anytime | Vitamin C source | None | Vitamin C helps collagen synthesis |
| Fish Oil | With meals | Food containing fat | None | Reduces fishy aftertaste; improves absorption |
Split your calcium dose: If you supplement with more than 500 mg of calcium, split it into two doses taken at different meals. Your body can only absorb about 500 mg at once. Taking 1,000 mg all at once means you’ll excrete much of it.
Take D3 and K2 with your fattiest meal: These fat-soluble vitamins absorb best when consumed with dietary fat. Morning eggs or avocado toast? Perfect. Take them then.
Magnesium at bedtime: Many people find magnesium glycinate helps them sleep better. It promotes muscle relaxation and calms the nervous system. Taking it at night serves double duty—supporting bones and improving sleep.
Separate calcium and magnesium: These minerals compete for the same absorption pathways. Taking them together means you’ll absorb less of both. Space them at least two hours apart for best results.
Watch for medication interactions: Calcium supplements can interfere with thyroid medications, certain antibiotics, and bisphosphonates (osteoporosis drugs). Take calcium at least four hours away from these medications. Ask your pharmacist about specific timing.
Bone-Building Meals: What This Actually Looks Like
Knowing which nutrients you need is one thing. Figuring out how to eat them is another. Here are practical meal ideas that pack multiple bone-supporting nutrients into each dish.
Breakfast: Collagen-Boosted Smoothie Bowl
Start your day with this nutrient-dense bowl that combines protein, calcium, and bone-building vitamins in one satisfying meal.
- 1 cup plain Greek yogurt (450 mg calcium, 20g protein)
- 1 scoop collagen peptides (10g protein)
- 1/2 cup mixed berries (vitamin C for collagen synthesis)
- 2 tablespoons chia seeds (180 mg calcium, 100 mg magnesium)
- Handful of spinach (vitamin K, calcium)
- 1 tablespoon almond butter (healthy fats, magnesium)
Total nutrients: ~630 mg calcium, 30g protein, plus vitamins C and K
Blend everything until smooth. Top with nuts, seeds, or coconut flakes. The combination of dairy calcium, collagen protein, and vitamin C creates a bone-building powerhouse that tastes like dessert. The healthy fats from almond butter help you absorb fat-soluble vitamins if you’re taking your D3 and K2 supplement with this meal.
Lunch: Sardine and White Bean Salad
This Mediterranean-inspired lunch delivers serious nutrition in a simple, flavorful package that takes minutes to prepare.
- 1 can sardines with bones (325 mg calcium, vitamin D, omega-3s, 23g protein)
- 1 cup white beans (160 mg calcium, 120 mg magnesium, 15g protein)
- Mixed greens (vitamin K)
- Cherry tomatoes (vitamin C)
- Olive oil and lemon dressing (helps absorb fat-soluble vitamins)
- Sprinkle of sesame seeds (additional calcium)
Total nutrients: ~500 mg calcium, 38g protein, plus vitamin D and K
If sardines aren’t your thing, substitute canned salmon or mackerel. The bones in canned fish are soft and edible—they’re the calcium jackpot many people overlook. The omega-3 fatty acids provide anti-inflammatory benefits that may help preserve bone density.
Dinner: Salmon with Sesame-Crusted Greens
This dinner covers all your bone-health bases while delivering restaurant-quality flavor at home.
- 6 oz wild salmon (vitamin D, 34g protein, omega-3s)
- 2 cups cooked collard greens (540 mg calcium, vitamin K)
- 1 tablespoon tahini (64 mg calcium, magnesium)
- 1 tablespoon sesame seeds (88 mg calcium)
- Medium sweet potato (magnesium, potassium)
- Side of quinoa (magnesium, protein)
Total nutrients: ~690 mg calcium, 45g protein, excellent vitamin D and K
Sauté the collard greens with garlic, then toss with tahini and sesame seeds before serving. The fat from salmon and tahini helps you absorb vitamins D and K. The combination of greens, seeds, and tahini delivers calcium in multiple forms your body can use efficiently.
Snacks That Build Bones
Between meals, reach for these calcium-rich options that keep your energy steady while supporting bone health.
- 1 oz almonds + 1 oz cheddar cheese: 375 mg calcium
- Fortified plant milk latte: 450 mg calcium
- Kefir with berries: 300 mg calcium plus probiotics
- Hard-boiled egg + orange: protein and vitamin C
- Edamame: protein, calcium, magnesium
One day of eating like this gets you close to 2,000 mg of calcium from food alone—well above most people’s needs. Add targeted supplementation only where gaps remain.
Understanding Your Bone Health
Bone mineral density matters, but it’s not the whole story. Your skeleton is living tissue engaged in a constant cycle of breakdown and renewal that continues throughout your life.
The bone remodeling cycle works like this:
Specialized cells called osteoclasts break down old bone tissue. This process, called resorption, releases minerals into your bloodstream. Then osteoblasts move in and build new bone to replace what was removed. This entire cycle takes about three to six months to complete in any given section of bone.
In healthy adults, these processes balance. The amount of bone removed equals the amount built. Your skeleton maintains its strength and density. But after age 30, the balance tips slightly. You lose a bit more than you build each year—about 0.5% to 1% annually under normal circumstances. Women experience rapid bone loss in the first five to seven years after menopause when estrogen drops sharply, losing up to 3% to 5% per year during this critical window.
This is why you can’t see results overnight. Supplements support the bone-building side of this cycle, but the actual remodeling takes months. DEXA scans typically show measurable changes only after 12 to 24 months of consistent intervention.
Fracture risk depends on more than density alone:
Bone quality matters as much as quantity. Strong bones have a healthy collagen matrix, proper mineralization, and good microarchitecture—the internal structure that gives bones strength and flexibility. Two people with identical bone density scores can have different fracture risks based on bone quality factors that DEXA scans don’t measure.
Your doctor might calculate your FRAX score—a tool that estimates your 10-year fracture risk based on bone density, age, sex, previous fractures, family history, and other factors. This score helps determine whether you need medication beyond supplements. A high FRAX score means your fracture risk exceeds what your bone density alone would suggest.
Trabecular vs. cortical bone:
Your skeleton contains two types of bone with different characteristics and functions. Trabecular bone (also called spongy bone) fills the interior of bones like the spine and hip. It’s metabolically active and responds quickly to changes—good or bad. This is where you see the fastest bone loss after menopause or with corticosteroid use.
Cortical bone forms the hard outer shell of all bones. It’s denser and changes more slowly. Cortical bone provides most of your skeleton’s structural strength, while trabecular bone handles metabolic functions and provides flexibility.
Osteoporosis affects trabecular bone first, which is why spine fractures often occur before hip fractures. Different supplements and interventions affect these bone types differently. Vitamin K2, for example, shows particularly strong effects on lumbar spine density—an area rich in trabecular bone.
The Hormone Connection: Why Menopause Changes Everything
Estrogen is one of your skeleton’s best friends. This hormone tells osteoclasts to slow down, protecting you from excessive bone breakdown. It also helps your intestines absorb calcium more efficiently and tells your kidneys to conserve it rather than excrete it in urine.
When estrogen drops during menopause, osteoclasts go into overdrive. Bone breakdown accelerates while bone building continues at the same pace. The result? Rapid bone loss that can be alarming. Women can lose up to 20% of their bone density in the five to seven years following menopause—a critical period when intervention matters most.
This is why post-menopausal women face the highest osteoporosis risk. The average woman reaches menopause around age 51. By age 65, about 25% of women have osteoporosis. By age 75, nearly half do. These numbers explain why bone health becomes so critical during and after the menopausal transition.
Men don’t experience the same dramatic hormonal shift, but testosterone gradually declines with age starting around age 30. Testosterone supports bone health in men similarly to how estrogen protects women. Lower testosterone correlates with reduced bone density and increased fracture risk, though men typically develop osteoporosis 10 to 15 years later than women.
Some men convert testosterone to estrogen through an enzyme called aromatase. This conversion helps maintain their bone density. Men with very low estrogen levels (yes, men need some estrogen) face higher fracture risk regardless of their testosterone levels.
What this means for supplementation:
Post-menopausal women benefit most from aggressive bone-health strategies. If you’re within 10 years of menopause, now is the time to optimize your nutrition and supplementation. The bone loss happens fast during this window, but it’s also when intervention has the greatest impact.
Hormone replacement therapy (HRT) can help preserve bone density during menopause, but it carries risks and benefits that you need to discuss with your doctor. Supplements support bone health whether or not you choose HRT, and many women use both approaches together for maximum protection.
Budget-Friendly Bone Health: Getting the Most from Your Money
Quality supplements aren’t cheap. But you can prioritize spending based on what matters most and where you’ll get the biggest return on investment.
Monthly Cost Comparison
| Approach | Monthly Cost | Pros | Cons |
|---|---|---|---|
| Food-only approach | $60-100 extra | Best absorption, whole food benefits, no pill burden | Requires meal planning, may not meet needs if intake is very low |
| Basic supplement stack | $25-40 | Convenient, consistent dosing, fills gaps | Quality varies by brand, less synergistic than food |
| Premium supplements | $60-90 | Higher quality forms, third-party tested, better absorption | More expensive, may exceed budget |
| Combination approach | $40-70 | Balanced and flexible, leverages both food and supplements | Requires planning and tracking |
If you can only afford one supplement: Make it vitamin D3 with K2. Deficiency in vitamin D is common and impairs calcium absorption no matter how much calcium you consume. A three-month supply of quality D3+K2 costs about $20-30—less than $10 per month.
If you can afford two: Add magnesium glycinate. These three supplements (D3, K2, magnesium) create the foundation for bone health by supporting calcium absorption, directing calcium to bones, and activating vitamin D. Total cost: about $30-35 monthly.
If you can afford three: Add collagen peptides if you’re post-menopausal or have diagnosed bone loss. A month’s supply of quality collagen runs $25-40, bringing your total to around $60-75 monthly.
Calcium from food beats calcium from pills: A gallon of fortified plant milk costs about $4 and provides 1,800 mg of calcium (plus added vitamin D). A month’s supply of calcium supplements costs roughly the same but lacks the complete nutrition whole foods provide. Prioritize food sources, supplement only to fill remaining gaps.
Generic vs. brand name: For basic supplements like magnesium citrate or vitamin D3, generic versions work fine if they’re third-party tested. The active ingredients are identical. For specialized supplements like collagen peptides or vitamin K2 (MK-7), quality matters more. The form and processing affect absorption and effectiveness, so investing in reputable brands makes sense.
What to Look for in Quality Supplements
Not all supplements deliver what their labels promise. The supplement industry is loosely regulated, which means quality varies dramatically between brands. Here’s how to choose wisely and avoid wasting money on inferior products.
| What to Look For | Why It Matters |
|---|---|
| Third-party tested (USP, NSF, ConsumerLab) | Independent verification ensures purity, potency, and absence of contaminants like heavy metals |
| D3 (cholecalciferol) not D2 | D3 is more effective at raising blood levels and maintaining them over time |
| K2 as MK-7 not MK-4 | MK-7 has a longer half-life, stays in your system longer, needs less frequent dosing |
| Magnesium glycinate or citrate | Better absorption than magnesium oxide; gentler on digestion with fewer laxative effects |
| Hydrolyzed collagen peptides | Broken down into smaller peptides for better absorption and utilization by your body |
| Oil-based D3+K2 capsules | Fat-soluble vitamins absorb better when dissolved in oil rather than pressed into dry tablets |
Third-party testing matters because the FDA doesn’t approve supplements before they hit shelves. Companies can make claims without proving them. Independent labs verify that bottles contain what labels claim—no more, no less—and test for heavy metals, microbes, and other contaminants that shouldn’t be there.
Look for seals from USP (United States Pharmacopeia), NSF International, or ConsumerLab on the bottle. These organizations set quality standards and test products regularly. If a supplement doesn’t display one of these seals, check the company’s website to see if they publish third-party test results.
What Doesn’t Work: Save Your Money
Not everything marketed for bone health deserves your dollars. Some supplements lack evidence. Others might cause more harm than good.
Trace minerals like boron and silicon: Yes, they play roles in bone metabolism. Animal studies show benefits. But evidence for supplementing beyond what you get from a varied diet is weak and inconsistent in humans. Unless you have a diagnosed deficiency, you’re probably fine without them.
Multiple nutrition reviews acknowledge that trace minerals contribute to bone health, but the research doesn’t support routine supplementation for most people. Focus on the big players first—calcium, vitamin D, K2, magnesium, and protein.
Strontium: Here’s a concerning one. Strontium citrate supplements can artificially inflate your DEXA scan results, making your bones appear denser than they actually are. Strontium atoms are heavier than calcium, so they show up brighter on scans. This creates a false sense of security that could delay needed treatment.
Additionally, some forms of strontium (particularly strontium ranelate, used in Europe but not approved in the US) have raised cardiovascular safety concerns, including increased risk of blood clots and heart attacks. Proceed with extreme caution and only under medical supervision if considering strontium.
Coral calcium: Despite marketing claims suggesting it’s superior to regular calcium, coral calcium offers no advantage over standard calcium supplements. It’s significantly more expensive with no additional benefit. Some coral calcium products have tested positive for lead contamination—exactly what you don’t want when trying to build healthy bones.
Mega-dosing anything: More is not better when it comes to bone supplements. High doses of calcium (above 2,000 mg daily from all sources) increase kidney stone risk and may raise cardiovascular concerns. Excessive vitamin D (above 10,000 IU daily without medical supervision) can cause toxicity, leading to nausea, weakness, kidney damage, and dangerous calcium buildup in soft tissues.
Excessive vitamin A (over 10,000 IU daily from retinol forms, not beta-carotene) actually increases fracture risk by interfering with bone formation. Stick to recommended ranges unless a healthcare provider advises otherwise based on lab work showing deficiency.
Single-nutrient thinking: Your bones need multiple nutrients working together in harmony. Calcium alone doesn’t build bones. Vitamin D alone has limited effects. The synergy between nutrients matters more than any single supplement. This is why comprehensive approaches that address multiple nutritional needs consistently outperform single-nutrient interventions.
Red Flags: When Supplements Aren’t Enough
Sometimes diet and supplements can’t solve the problem alone. Your body might be losing bone faster than nutrition can rebuild it. Watch for these warning signs that you need medical attention beyond supplements.
- You’ve lost more than 1.5 inches in height (suggests vertebral compression fractures)
- You broke a bone from a minor fall or bump (fragility fracture)
- You have severe, persistent back pain (could indicate spinal fractures)
- You’re taking medications that affect bone health long-term
- Your DEXA scan shows osteoporosis (T-score below -2.5)
- You have multiple risk factors and your FRAX score indicates high fracture risk
Medications that deplete bone density:
Several common medications accelerate bone loss, and knowing about them helps you take protective action early.
- Corticosteroids (prednisone, cortisone) used for more than three months
- Proton pump inhibitors (omeprazole, esomeprazole) taken long-term
- Some anti-seizure medications (phenytoin, carbamazepine)
- Certain breast cancer treatments (aromatase inhibitors like anastrozole)
- High doses of thyroid hormone replacement
- Depo-Provera birth control injections
- Some diabetes medications (thiazolidinediones)
- Certain antidepressants (SSRIs at high doses)
If you take any of these long-term, talk with your doctor about bone-protective strategies. You might need prescription osteoporosis medication beyond supplements. Don’t wait for bone loss to show up on a scan—prevention is easier than reversal.
When to see an endocrinologist:
Your primary care doctor can order DEXA scans and prescribe basic osteoporosis medications like bisphosphonates. But consider seeing an endocrinologist (hormone and bone specialist) if:
- You have osteoporosis before age 50 (suggests secondary causes)
- Your bone loss is progressing rapidly despite treatment
- You have secondary causes of bone loss (hyperparathyroidism, hyperthyroidism, Cushing’s syndrome)
- You’ve had fragility fractures despite normal or near-normal bone density
- Standard treatments aren’t working or you’re having side effects
Endocrinologists specialize in complex bone metabolism disorders. They can run additional tests to identify why your bones are losing density and recommend specialized treatments like teriparatide (bone-building medication) or denosumab (strong bone-loss prevention).
Your Action Plan: The Bone-Health Stack That Actually Works
Here’s how to put this together, step by step, without feeling overwhelmed by too many changes at once.
Step 1: Start with food
Track your calcium intake for three days using a food diary or app. Write down everything you eat and look up the calcium content. If you consistently hit 800-1,000 mg from food, you’re in good shape. If you’re falling short, identify where you can add calcium-rich foods without completely overhauling your diet.
Aim for 20 to 30 grams of protein per meal, spread throughout the day rather than loading it all at dinner. Choose protein sources that also provide calcium when possible: Greek yogurt, cheese, sardines, fortified plant milks, tofu. This dual-purpose approach makes hitting your targets easier.
Step 2: Core supplements
Take vitamin D3 paired with K2. Choose oil-based capsules or liposomal forms for better absorption since both are fat-soluble vitamins. Take them with your fattiest meal of the day—breakfast with eggs or avocado works perfectly.
Typical doses: 2,000 to 4,000 IU of D3 with 100 to 200 mcg of K2 (MK-7 form). Get your vitamin D level tested after three months to confirm you’ve reached the optimal range (30-50 ng/mL). Adjust your dose based on results.
Step 3: Add magnesium
Take 300 to 400 mg of magnesium glycinate or citrate, ideally in the evening about an hour before bed. This supports vitamin D activation, contributes to bone structure, and helps many people sleep better—a triple benefit.
Space magnesium at least two hours away from calcium supplements if you take both. The evening timing naturally creates this separation if you take calcium with meals.
Step 4: Consider collagen
If you’re post-menopausal or have diagnosed low bone density, mix 10 to 20 grams of collagen peptides into your morning coffee or smoothie. This supports the bone matrix that minerals build upon. Collagen is tasteless and dissolves completely in both hot and cold liquids.
Add a vitamin C source (berries, citrus, bell peppers) to the same meal to help your body synthesize collagen more efficiently.
Step 5: Fill the calcium gap if needed
If your diet consistently falls 300-500 mg short of your target after tracking for several days, add a modest calcium supplement. Take 500 mg or less per dose (split larger amounts across two meals) with food for better absorption.
Take calcium at least four hours away from thyroid medications, iron supplements, or osteoporosis drugs to avoid interactions that reduce effectiveness of either the supplement or the medication.
At a Glance: Your Daily Bone-Health Checklist
Print this and stick it on your fridge as a daily reminder:
Morning:
- Take D3 + K2 with breakfast (include healthy fats like eggs, avocado, or nuts)
- Add collagen to coffee or smoothie (if using)
- Eat protein-rich breakfast (aim for 25-30g)
Afternoon:
- Take calcium supplement with lunch if needed (max 500mg per dose)
- Choose calcium-rich snacks between meals (cheese, yogurt, fortified plant milk)
Evening:
- Take magnesium glycinate 1-2 hours before bed
- Eat protein-rich dinner (aim for 25-30g)
- Second calcium dose with dinner if needed
Weekly:
- Weight-bearing exercise 3-4 times (walking, dancing, hiking, tennis)
- Strength training 2-3 times (builds muscle that strengthens bones through mechanical loading)
Quarterly:
- Review your supplement routine and assess what’s working
- Check in with your doctor about any concerns
- Restock quality supplements before you run out
Yearly:
- Get vitamin D levels tested to ensure you’re in optimal range
- DEXA scan if you’re post-menopausal, over 65, or have risk factors
- Discuss bone health with your doctor and review your FRAX score
Conclusion
Your skeleton replaces itself completely about every ten years through the constant remodeling process. But measurable changes in bone density take months to years of consistent effort. Don’t expect miracles in six weeks or even six months.
The research is clear: calcium and vitamin D together form the foundation of bone health. Vitamin K2 helps direct calcium where it belongs instead of letting it deposit in arteries. Magnesium activates vitamin D and supports bone structure. Collagen provides the framework minerals build upon. Protein supports both muscle and bone through multiple mechanisms.
These nutrients work together in synergy. No single supplement creates strong bones. The interaction between nutrients matters as much as the nutrients themselves.
Start with food. A diet rich in dairy or fortified alternatives, leafy greens, fish with bones, nuts, seeds, and adequate protein covers many of your needs naturally. Add targeted supplementation to fill remaining gaps based on your actual intake, not assumptions.
Get tested. Know your vitamin D level through blood work. Consider a DEXA scan if you have risk factors or you’re post-menopausal. Use data to guide decisions instead of guessing what you might need.
Be patient. Bone health is a long game measured in years, not weeks. Consistency beats intensity every time. Taking supplements sporadically won’t help. Taking them daily for months and years will.
FAQs
Can you rebuild bone density naturally?
Yes, but with realistic limits. You can slow bone loss and make modest improvements in bone density through nutrition, supplements, and weight-bearing exercise. Studies show increases of 1-3% are realistic over one to two years with consistent intervention—meaningful gains that reduce fracture risk.
If you already have osteoporosis (not just osteopenia), you’ll likely need prescription medication along with lifestyle changes. Supplements alone can’t reverse advanced bone loss, but they support whatever treatment approach your doctor recommends and help maximize medication effectiveness.
How long does it take for bone supplements to work?
The bone remodeling cycle takes three to six months to complete in any given area of your skeleton. Measurable changes in bone density typically show up after 12 to 24 months of consistent supplementation and lifestyle changes. This timeline reflects the biological reality of how bone forms.
You might notice other benefits sooner. Many people report better energy and fewer muscle cramps within weeks of correcting vitamin D or magnesium deficiency. Joint comfort may improve within months of starting collagen. But bone density changes take patience and consistency.
What’s the best form of calcium to take?
Calcium citrate absorbs well with or without food and causes less digestive upset than calcium carbonate. If you take proton pump inhibitors or have low stomach acid (common in older adults), calcium citrate is your best choice because it doesn’t require acid for absorption.
Calcium carbonate provides more elemental calcium per pill (making it more cost-effective) but requires stomach acid for absorption. Take it with meals to maximize absorption and minimize digestive discomfort.
Both forms work when used correctly. Choose based on your digestion, medication use, and when you prefer to take supplements.
Should I take calcium if I eat dairy?
Calculate your actual calcium intake first before adding supplements. One cup of yogurt plus one ounce of cheese gives you about 750 mg. If you eat these amounts daily plus other calcium sources (leafy greens, fortified foods, nuts), you might hit 1,000-1,200 mg from food alone.
Many people overestimate how much dairy they eat. Track it honestly for three days using actual measurements, not guesses. If you’re consistently 300-400 mg short of your target, add a modest supplement. If you’re meeting your needs through food, additional calcium won’t help and might cause problems.
Can you take too much vitamin D?
Yes. Vitamin D toxicity causes nausea, vomiting, weakness, confusion, and dangerous calcium buildup in your blood and organs. But it takes very high doses sustained over time—usually above 10,000 IU daily for months.
Staying below 4,000 IU daily is safe for most adults without medical supervision. Higher doses (10,000 IU or more) should only be taken under medical supervision with regular blood testing to monitor levels and calcium.
More isn’t better with vitamin D. Get tested and dose appropriately based on your actual blood levels, not guesswork.
Do collagen supplements really strengthen bones?
Recent research says yes, particularly for post-menopausal women who face the highest bone loss risk. Multiple studies show that specific hydrolyzed collagen peptides improve bone mineral density at the spine and hip when taken consistently for 6-12 months.
Collagen provides the structural framework your bones mineralize around. It won’t replace calcium and vitamin D, but it appears to offer additional benefits beyond minerals alone. The combination of collagen plus calcium and vitamin D shows better results than minerals alone in several studies.
What medications hurt bone health?
Corticosteroids top the list. Taking prednisone or similar drugs for more than three months significantly increases bone loss and fracture risk, sometimes dramatically. If you need long-term corticosteroids, talk with your doctor about bone protection strategies immediately.
Proton pump inhibitors (PPIs like omeprazole) reduce calcium absorption when taken long-term. Some seizure medications, diabetes drugs, and cancer treatments also affect bones. Depo-Provera birth control shots reduce bone density, especially in young women.
If you take any medication long-term, ask your doctor about bone health effects and whether you need additional monitoring, supplements, or protective treatments.
At what age should I start taking bone supplements for osteoporosis prevention?
It depends on your risk factors more than your age alone. Post-menopausal women should assess their bone health and likely need supplementation during the critical window when bone loss accelerates. Men over 70 face increased risk and should consider supplementation.
But younger people with risk factors (family history, medications, digestive disorders, very low body weight, early menopause) should start earlier. Get a DEXA scan if you have multiple risk factors or you’re a woman past menopause. Let the results guide your decision rather than age alone.
Prevention is easier than reversal. Don’t wait until you break a bone to start thinking about bone health.


