We’ve done the research for you. This guide ranks 20 popular liver supplements into four clear groups based on real human studies. Some have strong proof. Others are just starting to show promise. A few shouldn’t be used at all.
Before you start anything new: Talk to your doctor first. This is especially true if you already have liver problems. Supplements can interact with medications and may not be safe for everyone.
Understanding Your Liver Condition
Before picking a supplement, you need to know what’s actually happening with your liver. Different conditions need different approaches.
Fatty Liver Disease (NAFLD)
NAFLD means fat builds up in your liver cells. Most people have no symptoms. You might find out you have it during a routine ultrasound or blood test.
NAFLD comes in two forms. Simple fatty liver (steatosis) means fat is there but no inflammation is happening. This is the earlier stage. It’s also more likely to improve with lifestyle changes.
NASH (Nonalcoholic Steatohepatitis)
NASH is the serious cousin. Your liver has fat AND inflammation. Think of it like rust developing on metal. The inflammation can damage liver cells and lead to scarring over time.
Not everyone with fatty liver develops NASH. But if you do, supplements become more critical alongside medical care. NASH affects roughly 1-2% of people and is becoming more common.
Cirrhosis and Advanced Liver Disease
This is scarring so severe that your liver can’t function properly. Supplements alone won’t help here. You need medical treatment and specialist care.
Cholestatic Liver Disease (PBC and PSC)
These rare diseases affect bile flow. Bile gets stuck in the liver instead of moving to your intestines. This causes itching, yellowing of skin, and eventual scarring. These conditions require prescription medications. Supplements play only a supporting role.
Viral Hepatitis and Autoimmune Disease
Infection or immune problems damaging your liver are different from fatty liver. Treatment focuses on the root cause first. Supplements help but aren’t primary therapy.
Understanding Liver Tests
Your doctor will check several numbers to see how your liver is doing. Understanding these helps you track progress and spot problems early.
ALT and AST (Liver Enzymes)
ALT (alanine aminotransferase) and AST (aspartate aminotransferase) are proteins your liver releases when cells get damaged. Normal ranges vary by lab, but typically:
- ALT: 7-56 units per liter
- AST: 10-40 units per liter
High numbers mean liver cells are leaking or dying. They can spike from supplements, medications, or liver disease. Most supplements take 8-12 weeks to lower these numbers.
AST/ALT Ratio
Divide your AST by your ALT. This ratio tells your doctor what type of liver damage you have. In simple fatty liver, ALT is usually higher. When this ratio flips and AST becomes higher, it suggests scarring (cirrhosis) might be starting. This ratio matters more than either number alone.
Bilirubin
This orange-yellow pigment comes from old red blood cells. Your liver processes it and sends it out through bile. High bilirubin makes your skin and eyes yellow (jaundice). Normal is less than 1.2 mg/dL.
Albumin and Total Protein
Albumin is made by your liver. When liver function declines, albumin levels drop. This shows up as swelling in your legs and belly. Normal albumin is 3.5-5.0 g/dL.
Imaging: Ultrasound, Fibroscan, and MRI
Ultrasound shows if fat is in your liver. Fibroscan (transient elastography) measures stiffness. A stiffer liver suggests scarring. MRI is the most detailed but most expensive. These imaging tests usually improve over 12-24 weeks with the right supplements and lifestyle changes.
Testing Timeline
Get baseline tests before starting supplements. Retest at 3 months, then every 6 months if making progress. If numbers aren’t improving, your supplements may not be helping or your dose may be wrong.
🔍 Liver Symptom Checker
Identify your liver condition to find the right supplements
Tier 1: Strong Clinical Evidence
These supplements have passed rigorous human trials. They show major, measurable improvements—like actual tissue healing or life-saving effects.
1. Vitamin E (For One Very Specific Condition)
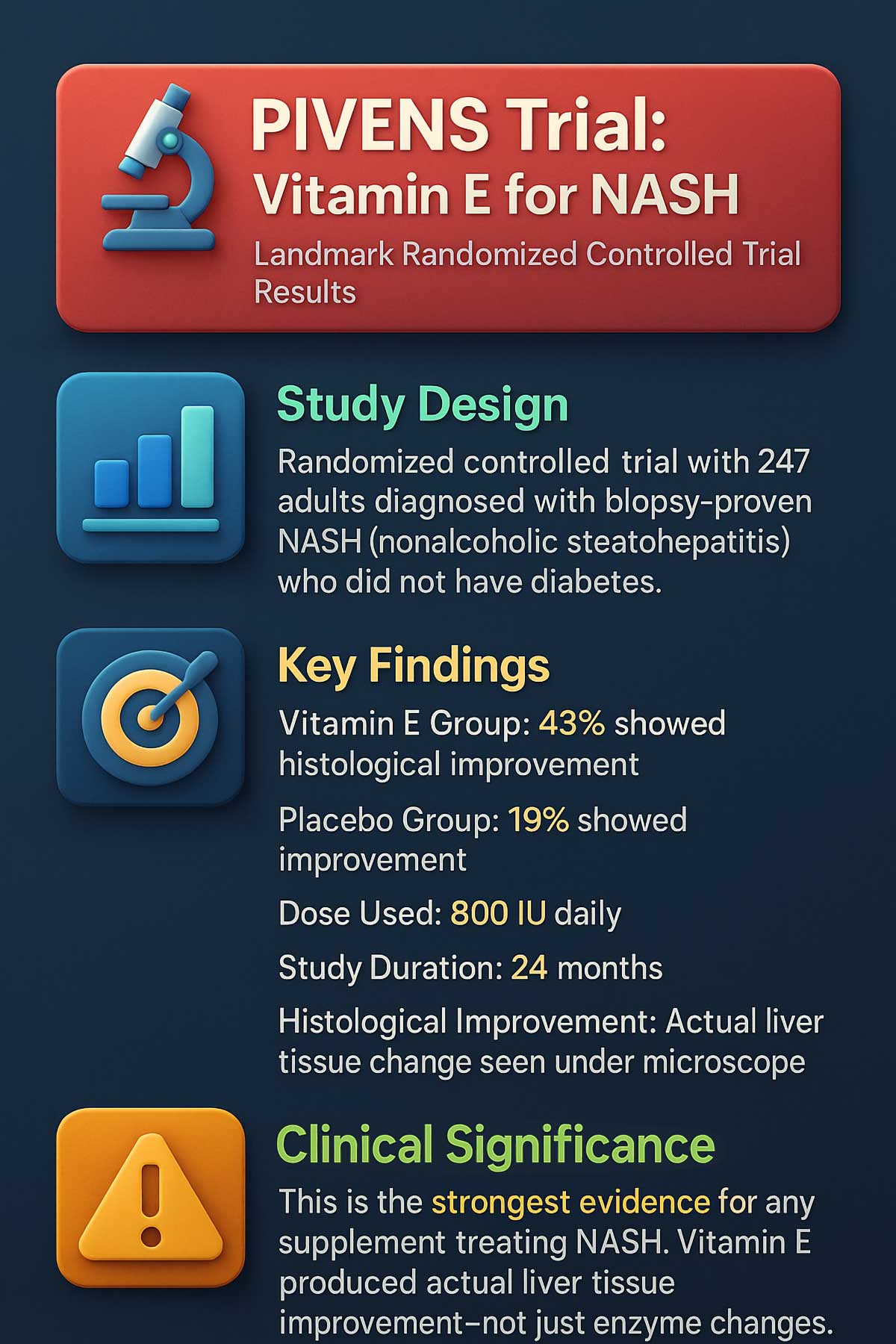
The Real Story: Vitamin E isn’t a catch-all liver fix. The research supports it for just one situation: adults without diabetes who have biopsy-proven NASH (fatty liver with inflammation).
The landmark PIVENS trial proved this. About 43% of people taking a specific dose of Vitamin E showed real tissue improvement. Compare that to 19% on placebo. This wasn’t just enzyme changes—researchers actually looked at liver tissue under a microscope and saw improvement.
Who Should Use It: Only people with confirmed non-diabetic NASH under a doctor’s supervision. If this isn’t you, skip it.
Typical Dose: 300-600 IU daily, but only under medical guidance.
Why You Need to Be Careful: More isn’t better with Vitamin E. Large studies show increased risk of death at doses of 400 IU per day or higher. Men taking Vitamin E also had higher rates of prostate cancer. This supplement requires medical oversight—period.
Not for Diabetics: If you have type 2 diabetes, Vitamin E won’t help your NASH and may cause harm. Your doctor will exclude you from this option.
2. N-Acetylcysteine (NAC)
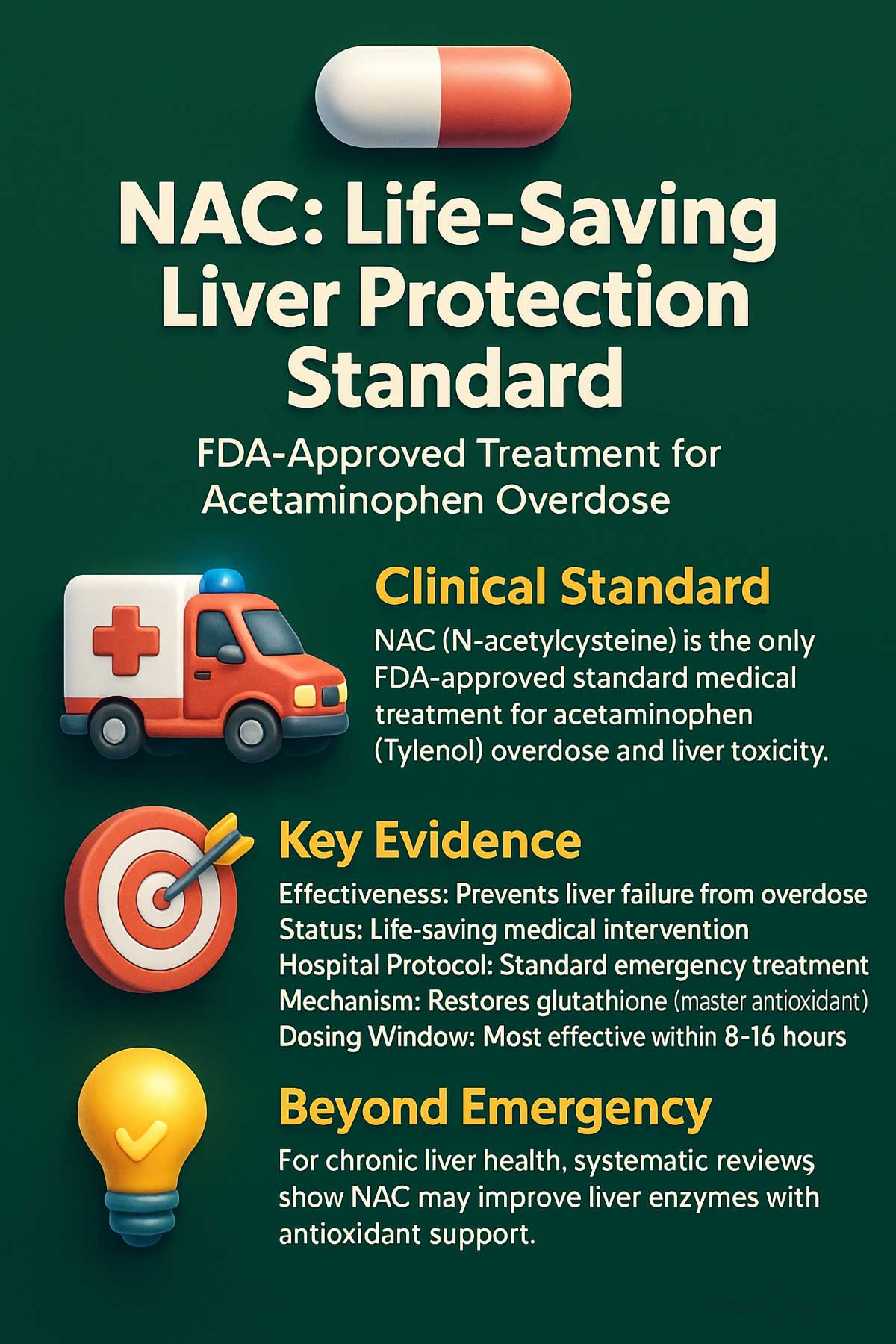
The Proof: NAC is the only standard medical treatment for acetaminophen (Tylenol) overdose. It saves lives by protecting the liver from serious damage. That’s not a supporting role—that’s life-saving proof.
When someone overdoses on Tylenol, NAC restores glutathione (a master antioxidant) and prevents liver failure. Hospitals keep this as emergency medication. No other supplement has this level of proven, critical effectiveness.
Beyond Emergencies: For ongoing liver health, the evidence is mixed but promising. Research reviews show NAC may help improve liver enzymes in chronic conditions like NAFLD thanks to its strong antioxidant power.
Who Benefits: NAC is essential for overdose treatment. It’s also reasonable to consider as a supportive supplement for general antioxidant protection if your doctor agrees.
Typical Dosing: Medical-grade NAC for general support usually ranges from 600–1,200 mg daily, but always follow your doctor’s recommendation.
Timing Matters: Take NAC on an empty stomach for better absorption. It tastes unpleasant, so many brands offer it in capsules.
Tier 2: Moderate Evidence
These supplements have consistent, positive results from multiple human studies. They improve liver enzymes, show up better on imaging, or reduce specific symptoms.
3. S-Adenosyl-L-Methionine (SAMe)
The Overlooked Option: SAMe has solid research behind it, but you don’t hear about it much. That’s because it doesn’t have the marketing buzz of trendy herbals.
What It Does: SAMe improves bile flow in cholestatic liver disease (bile gets stuck). Multiple controlled trials show it benefits patients with Primary Biliary Cholangitis and Primary Sclerosing Cholangitis. It also shows benefits for alcoholic liver disease in studies.
How It Works: SAMe is a compound your body makes from the amino acid methionine. It supports methylation reactions that keep liver cells healthy and help move bile out of your liver.
The Takeaway: This is real science with moderate backing. Ask your doctor about SAMe if you have bile flow issues or alcoholic liver disease.
Typical Dose: 1,200-1,600 mg daily, usually split into doses.
Possible Side Effects: Nausea, insomnia, and dry mouth are most common. Usually mild.
4. Milk Thistle (Silymarin)
The Famous Herb: Milk thistle is everywhere in liver supplement blends. Does it work?
Yes—but realistically. Multiple research reviews confirm that silymarin (the active compound) produces modest improvements in liver enzymes like ALT and AST in people with NAFLD. A 2024 meta-analysis of 19 studies found consistent but small improvements in liver function tests.
Set Your Expectations Right: Think of it as a supportive player, not a cure. It helps, but it’s not a game-changer by itself.
Typical Dose: 150–300 mg of silymarin daily is standard in research. Look for products standardized to 80% silymarin.
How It Works: Silymarin acts as an antioxidant and helps prevent liver cell damage. It also stimulates protein synthesis to help rebuild damaged cells.
Safety: Milk thistle is very safe. Minor GI upset is the only common side effect.

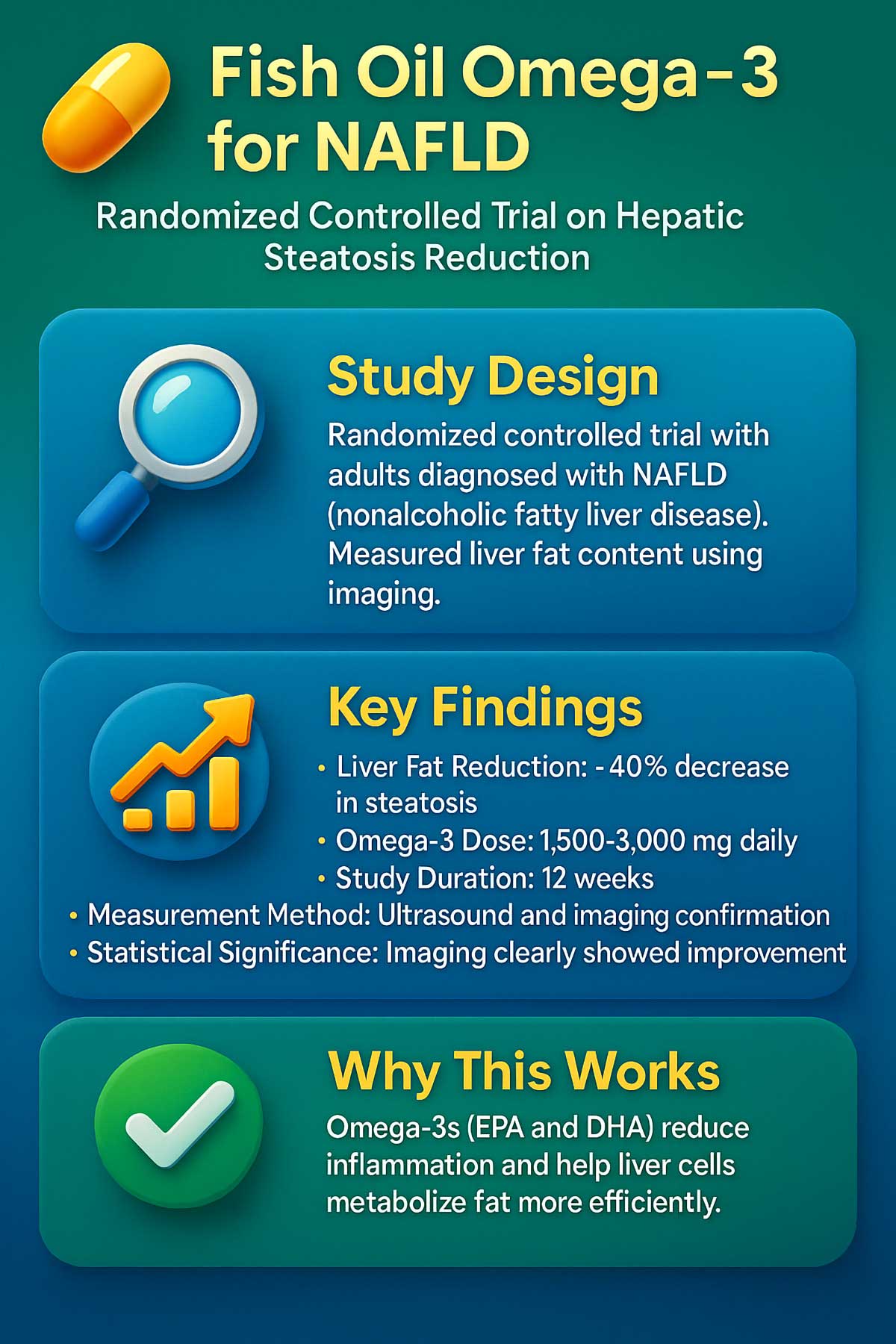
5. Omega-3 Fatty Acids (EPA/DHA)
The Research: Strong evidence from controlled trials and research reviews shows omega-3s genuinely reduce liver fat. Imaging studies prove it works.
A major randomized trial found that people taking fish oil with 1,500-3,000 mg of omega-3s daily reduced their liver fat content by roughly 40% over 12 weeks. That’s huge. The improvement showed up on ultrasound and other imaging.
Why It Works: Omega-3s, especially from fish oil, target the “fatty” part of fatty liver disease. They reduce fat storage in liver cells and decrease inflammation. If you have NAFLD and your imaging shows fat buildup, this is worth discussing with your doctor.
Where to Get Them: Fish like salmon, sardines, and mackerel are excellent. Fish oil supplements work too. The dose in studies typically ranges from 1,500–3,000 mg daily.
Taking It Right: Take fish oil with food to reduce fish burps. Quality matters—look for brands tested by third parties.
Caution: Fish oil can thin your blood. Tell your doctor if you’re on blood thinners like warfarin.
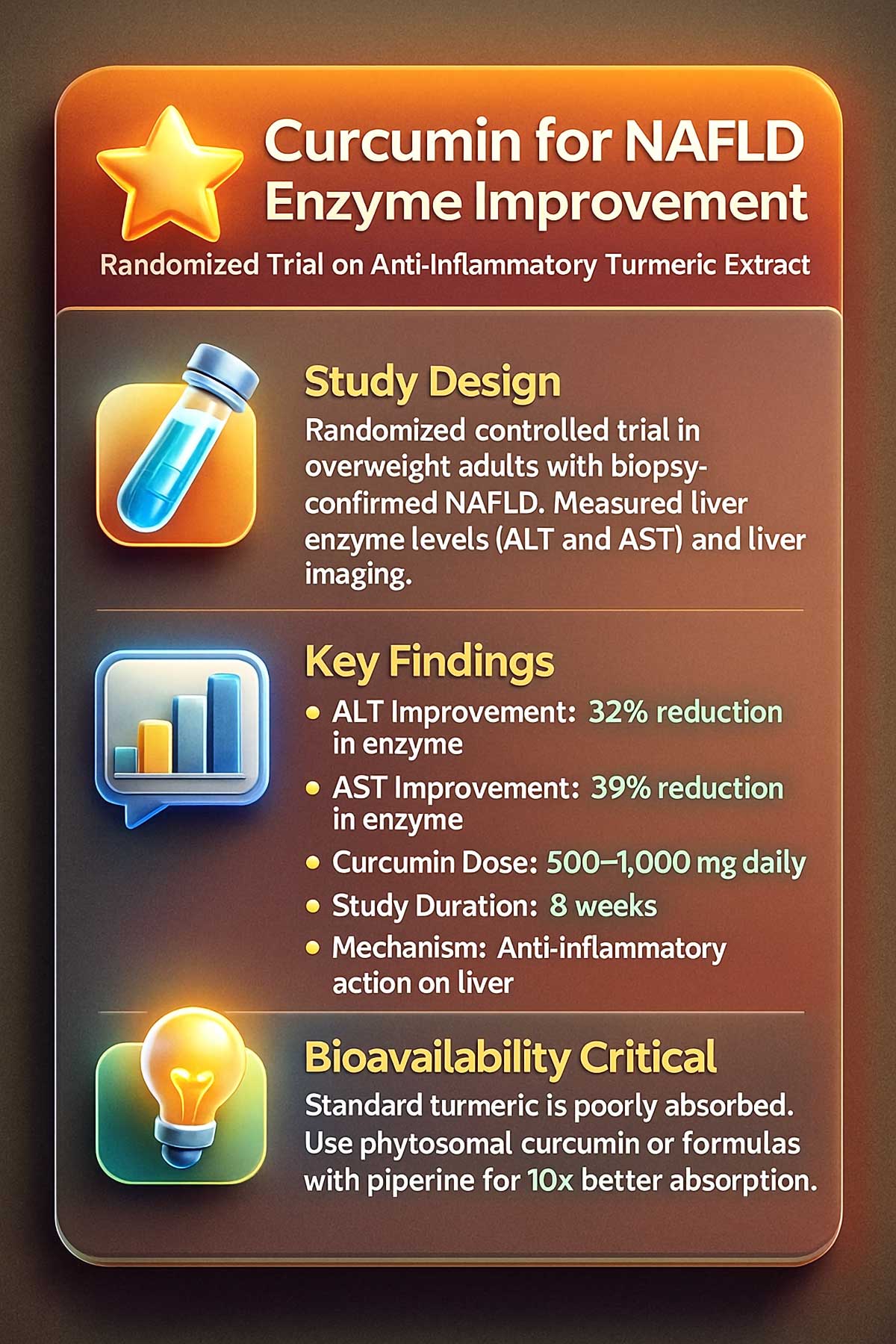
6. Curcumin (From Turmeric)
The Science: Several well-done controlled trials show curcumin reduces liver enzymes and improves liver imaging in NAFLD patients.
One study had overweight people with fatty liver take either curcumin or placebo for 8 weeks. The curcumin group showed 32% improvement in ALT levels and 39% improvement in AST levels. The imaging also improved.
The Catch: Standard turmeric powder has poor absorption. Your body can’t use most of it. Look for formulations with better absorption, like phytosomal curcumin or blends with piperine (a compound from black pepper).
Realistic Dosing: Studies used 500–1,000 mg daily of bioavailable curcumin, not plain turmeric powder from your spice rack.
Why Absorption Matters: Regular curcumin is fat-soluble, which means it doesn’t dissolve well in your digestive system. Only about 1% gets absorbed. Phytosomal curcumin (curcumin bound to special fats) boosts absorption to 30%.
Typical Timeline: Expect 8-12 weeks to see improvements in blood work.
7. Choline
The Link: Choline deficiency directly causes fatty liver. This is proven and clear. Without enough choline, your liver can’t move fat out of its cells.
The Gap: We don’t have many human studies yet on choline supplements for liver health. But the logic is solid: your liver needs choline to transport fats into packages that leave the cell.
Who Might Benefit: Anyone eating very little choline. It’s found in eggs, lean meat, fish, and soy. If your diet is low in these foods, choline supplementation makes sense. Talk to your doctor about the right dose.
Food Sources: 1 egg has about 125 mg of choline. 3 ounces of salmon has 56 mg. 1 cup of cooked broccoli has 63 mg. Most people need 425-550 mg daily.
Supplementation: If taking choline as a supplement, 500-1,000 mg daily is typical. Choline bitartrate is cheap but poorly absorbed. Alpha-GPC is better absorbed.
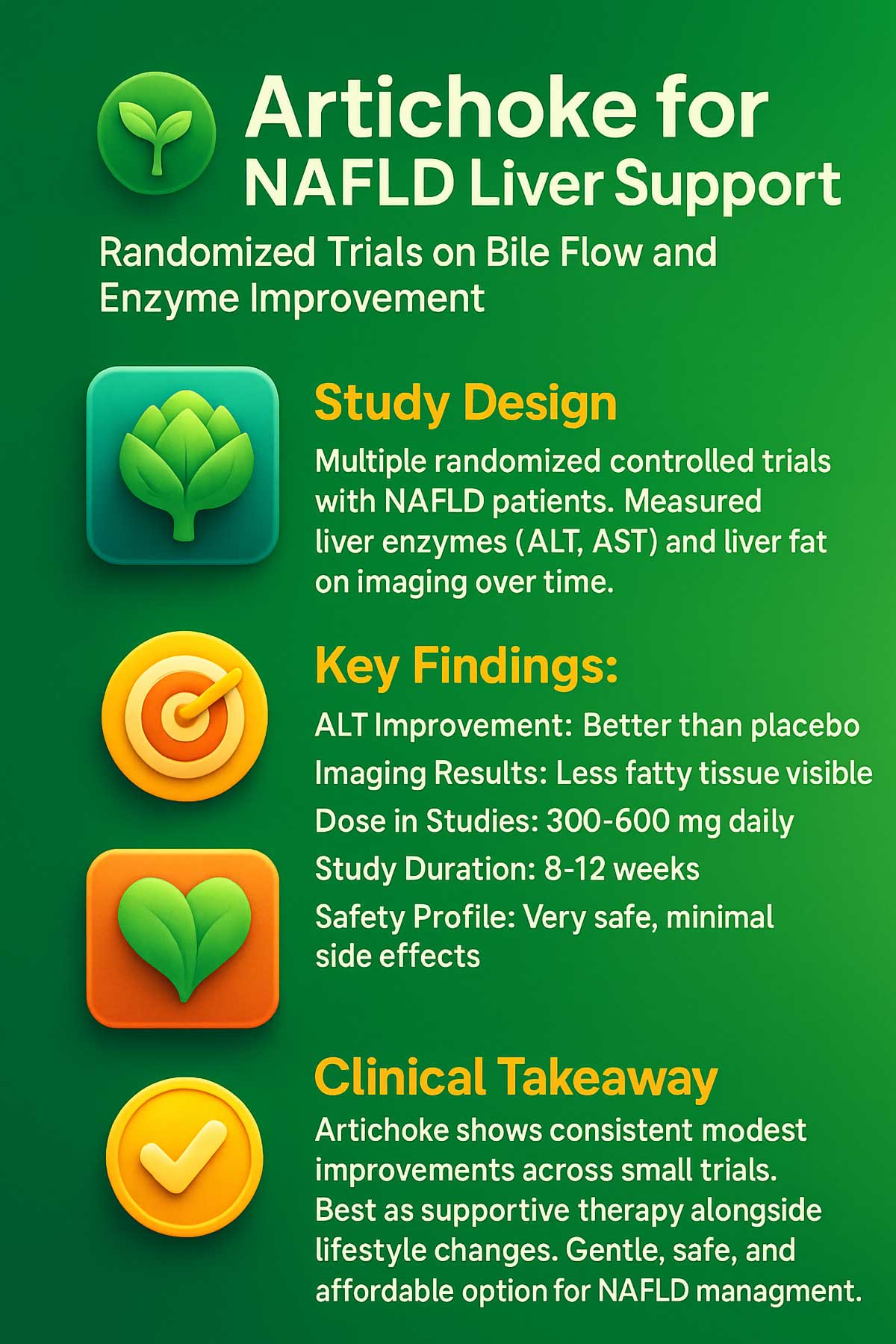
8. Artichoke Leaf Extract
The Evidence: Multiple small controlled trials show consistent improvements in liver enzymes for NAFLD patients.
How It Helps: Artichoke stimulates bile production and provides antioxidant protection. It’s a gentle, consistent supporter.
One study gave NAFLD patients either artichoke extract or placebo. After 12 weeks, the artichoke group had better ALT levels and less fatty tissue on imaging compared to placebo.
Typical Dose: Studies used 300–600 mg daily, usually split into doses.
Side Effects: Very rare. Mild stomach upset is possible if you’re sensitive to plants in the daisy family.
How It Works: Artichoke contains inulin and other compounds that support bile flow and reduce liver inflammation.
Tier 3: Limited or Emerging Evidence
These show early promise. The science is interesting, but we need more research before making strong recommendations.
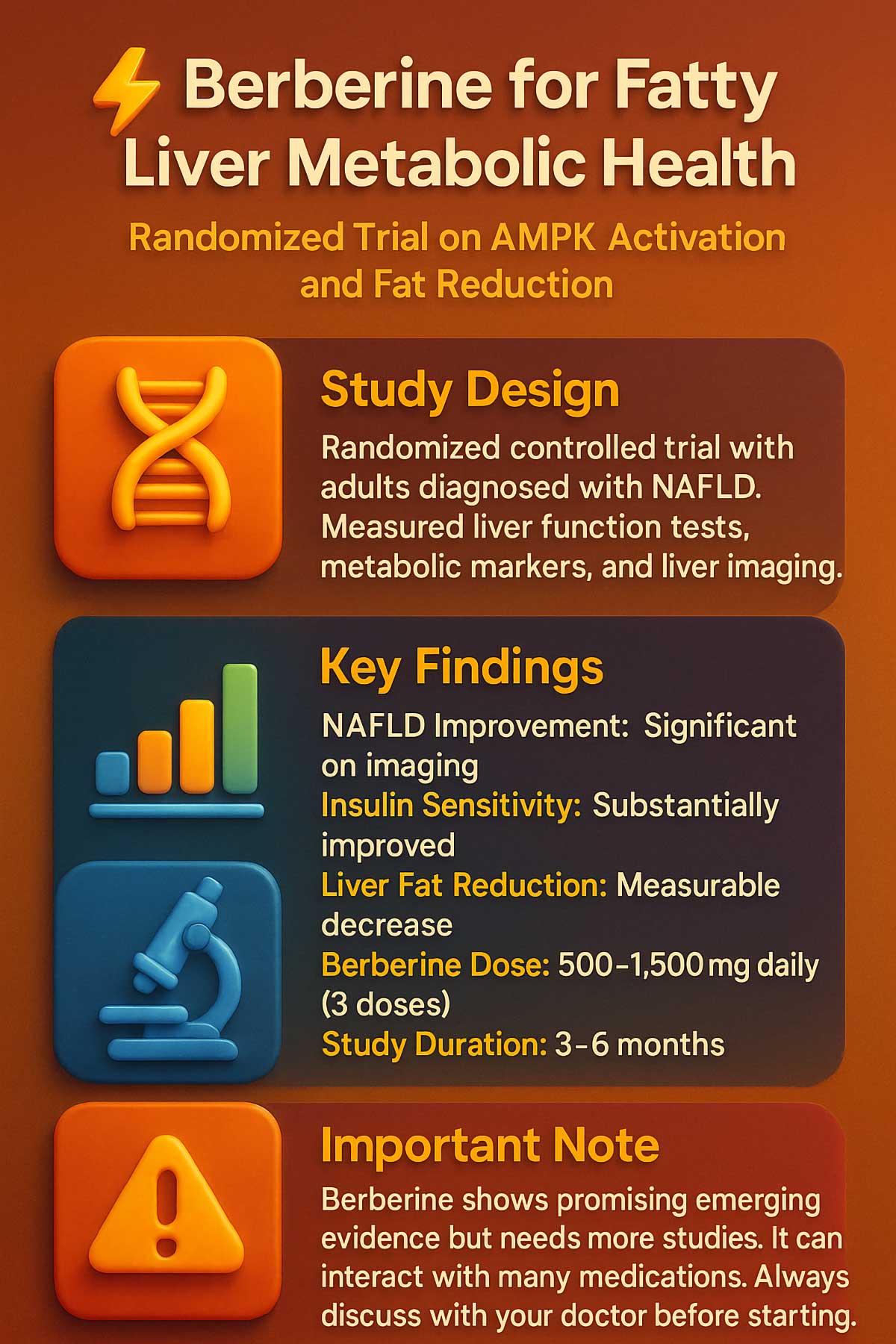
9. Berberine
The Potential: Berberine is a powerful compound that works through a mechanism called AMPK activation. Think of AMPK as your cellular energy manager. When activated, it tells your cells to burn fat instead of storing it.
One controlled trial had people with NAFLD take either berberine or placebo for 3 months. The berberine group showed improvements in liver enzymes, lower blood sugar, and reduced liver fat on imaging.
The Reality: We need more large studies. The early signal is good, but it’s not proven enough for strong recommendations yet.
Safety Note: Berberine can interact with medications. Always ask your doctor before starting.
Typical Dose: 500-1,500 mg daily, usually split into three doses.
10. Glycine
The Early Signal: One human pilot study found glycine improved markers of oxidative stress and liver function. The mechanism makes sense: glycine is a fundamental building block your liver uses for repair.
The Honest Truth: This is brand new to liver research. Much more work is needed before we know if it truly helps.
Possible Benefit: Your liver uses glycine to make glutathione, a master antioxidant. More glycine might mean more glutathione production.
Typical Dose: 3-5 grams daily in studies.
11. Alpha-Lipoic Acid (ALA)
What We Know: Small controlled trials show some benefit in NAFLD, but the studies are limited in size and quality.
Main Use: ALA is best known as a general antioxidant. Its liver-specific benefits remain modest compared to other options.
Typical Dose: 300-600 mg daily.
Timing: Take ALA on an empty stomach for better absorption.
12. Green Tea Extract (EGCG)
The Good News: Some studies show green tea compounds (catechins) can reduce liver fat.
The Critical Warning: This is important. High-dose green tea supplements carry real risk of severe liver injury. Concentrated extracts are riskier than drinking regular green tea.
Multiple cases of liver damage from high-dose green tea extract exist in medical literature. When concentrated, the catechins can stress the liver rather than help it.
The Smart Choice: Enjoy green tea as a beverage. Skip the supplement bottles at high doses. If you love green tea benefits, drink 2-3 cups daily instead of taking pills.
Safe Approach: If supplementing, stick to 200-400 mg daily maximum, which equals 2-3 cups of tea.
Tier 4: Weak or Conditional Evidence
These supplements have very limited human data for liver health. Some only work if you’re deficient. Most are supported mainly by lab studies, not human trials.
13. Garlic Extract
Small studies show positive signals for reducing liver fat, but the research is limited. More rigorous trials are needed.
Typical Dose: 400-1,200 mg daily of aged garlic extract.
14. Betaine
Early work suggests modest fat reduction in fatty liver. Not enough evidence yet to recommend widely.
Typical Dose: 500-2,000 mg daily.
How It Works: Betaine helps transport fats, similar to choline. The benefit might come from improved fat metabolism.
15. Vitamin C
Weak standalone evidence. It’s typically studied combined with Vitamin E, not alone.
Best Use: Get from food sources like citrus, berries, and bell peppers rather than supplements.
16. Zinc
Here’s the key: Zinc only helps if you’re deficient, which is common in chronic liver disease. If you have normal zinc levels, supplements won’t help. Get tested first.
When It Matters: Liver disease patients often lose zinc in urine. Deficiency causes problems with immunity and liver repair. Testing is simple and affordable.
Safe Dose: Don’t exceed 40 mg daily without medical guidance. Too much zinc blocks copper absorption.
17. Beetroot Extract
Very early pilot data exists. Not enough human evidence to recommend for liver disease.
Alternative: Eating whole beets provides fiber and antioxidants without concentration risks. Include them in your diet if you enjoy them.
18. Selenium
Use extreme caution. The safe dose range is very narrow. It only helps if you’re deficient. Too much can be harmful.
The Problem: Selenium has a therapeutic window of just a few micrograms. Below that, it doesn’t help. Above that, it becomes toxic. Getting tested before supplementing is non-negotiable.
Symptoms of Excess: Garlic breath, nail brittleness, neuropathy (nerve damage).
Safe Approach: Get selenium from food (Brazil nuts have lots of it) or only supplement under medical supervision with testing.
19. Dandelion Root
Popular in traditional medicine, but human evidence is currently insufficient. Most research is in lab studies, not people.
What We Know: Lab studies show it might help, but this hasn’t translated to proven human benefit yet.
20. Ursodeoxycholic Acid (UDCA)
Important Distinction: This is a medication, not a supplement.
UDCA is FDA-approved and highly effective for Primary Biliary Cholangitis (PBC). It significantly slows disease progression in this specific condition.
But clinical trials prove it doesn’t work for NAFLD. Don’t use it without a prescription and medical supervision. Using prescription medications as supplements is dangerous and ineffective.
Tier 4B: Only Use If Deficient
Vitamin D
Most people are deficient. Low vitamin D is linked to worse liver disease outcomes. But supplementation studies are still developing.
Best Approach: Get your level tested. If deficient (below 30 ng/mL), supplementation makes sense.
Typical Dose: 1,000-4,000 IU daily, adjusted based on your test results.
Condition-Specific Supplement Recommendations
Not all supplements work for all conditions. Here’s what the research shows for your situation.
For Simple NAFLD (Fatty Liver, No Inflammation)
Start with lifestyle changes first—they work best here. If adding supplements:
Priority Order:
- Omega-3 (fish oil 1,500-3,000 mg daily)
- Milk Thistle (150-300 mg daily)
- NAC (600-1,200 mg daily)
- Choline (500-1,000 mg daily, or eat more eggs and fish)
- Curcumin (500-1,000 mg daily with enhanced absorption)
Avoid: Vitamin E (not proven here), high-dose Green Tea Extract
For NASH (Fatty Liver with Inflammation, Non-Diabetic)
This is more serious. Supplements become more important alongside medical care.
Priority Order:
- Vitamin E (300-600 IU daily, only under medical supervision)
- NAC (600-1,200 mg daily)
- Omega-3 (1,500-3,000 mg daily)
- Curcumin (500-1,000 mg with enhanced absorption)
- Milk Thistle (150-300 mg daily)
Consider: SAMe if inflammation markers are very high
For NASH (If You Have Type 2 Diabetes)
Skip Vitamin E—it won’t help and carries risks.
Priority Order:
- NAC (600-1,200 mg daily)
- Berberine (500-1,500 mg daily, but ask doctor about interactions)
- Omega-3 (1,500-3,000 mg daily)
- Curcumin (500-1,000 mg with enhanced absorption)
- Alpha-Lipoic Acid (300-600 mg daily)
For Cholestatic Disease (PBC, PSC)
These conditions require prescription treatment first.
Supportive Supplements:
- SAMe (1,200-1,600 mg daily)
- NAC (600-1,200 mg daily)
- Milk Thistle (150-300 mg daily)
- Curcumin (500-1,000 mg with enhanced absorption)
Critical: These supplements support treatment but replace nothing. Stay on your prescribed medications.
For General Liver Support (No Diagnosis)
If you want to protect your liver but have no known disease:
Priority Order:
- NAC (600-1,200 mg daily)
- Milk Thistle (150-300 mg daily)
- Omega-3 (1,000-2,000 mg daily)
Keep It Simple: Don’t take 10 supplements. A few quality ones beats many mediocre ones. Focus on lifestyle first.
💊 Supplement Recommendation Engine
Get personalized supplement recommendations for your liver health
Step 1: What is your liver condition?
Step 2: Check for drug interactions
Select any medications you're currently taking
Step 3: What is your budget preference?
Step 4: Any dietary restrictions?
Lifestyle: The Non-Negotiable Foundation
Supplements help. Lifestyle changes heal.
This is the hardest truth to accept: no pill beats diet, movement, and weight loss. If you’re not addressing lifestyle, supplements are just expensive pee.
The Mediterranean Diet for Liver Health
The Mediterranean diet is the most studied and most effective eating pattern for liver health. It’s not strict or complicated.
The Structure:
- 40-50% carbohydrates (whole grains, beans, legumes)
- 25-30% healthy fats (olive oil, nuts, fish)
- 15-20% protein (fish, chicken, beans, not too much red meat)
- High fiber (vegetables, fruits, whole grains)
Key Principles:
Use olive oil as your main fat. It contains compounds that reduce liver inflammation. Aim for 2-3 tablespoons daily.
Eat fatty fish 2-3 times weekly. Salmon, sardines, mackerel, and trout contain omega-3s. These actually decrease liver fat on imaging.
Pile vegetables on every plate. Aim for 6-8 servings daily. Different colors provide different compounds. Dark leafy greens have the most antioxidants.
Choose whole grains over refined. Your liver prefers complex carbs. White bread and pasta spike blood sugar faster.
Limit red meat to once weekly. Choose lean poultry most days instead.
Add beans and legumes. Chickpeas, lentils, and beans have fiber that your gut bacteria love. Your gut health affects your liver.
Foods to Prioritize
Fish and Seafood: Salmon, sardines, mackerel, trout, halibut
Nuts and Seeds: Almonds, walnuts, chia seeds, flax seeds
Legumes: Lentils, chickpeas, black beans, white beans
Vegetables: Spinach, kale, broccoli, Brussels sprouts, bell peppers, tomatoes, carrots
Fruits: Berries, citrus, apples, pears (whole fruit, not juice)
Whole Grains: Oats, brown rice, quinoa, whole wheat bread and pasta
Herbs and Spices: Turmeric, garlic, oregano, basil
Healthy Oils: Extra-virgin olive oil, avocado oil
Foods to Limit
Fried Foods: These contain oxidized oils that stress your liver.
Processed Foods: Packaged snacks, deli meats, fast food. These have trans fats and excess sodium.
Refined Carbs: White bread, pastries, sugary cereal. These spike blood sugar and promote liver fat storage.
Added Sugars: Soda, juice, candy, desserts. Sugar is converted to fat in your liver.
Alcohol: Even moderate amounts worsen liver disease. Most people with liver disease should avoid it completely.
High-Fat Dairy: Full-fat cheese, whole milk, butter. Choose low-fat or plant-based options.
Weight Loss: The Most Powerful Intervention
Losing just 5-7% of your body weight significantly improves fatty liver disease. This isn’t about looking good—it’s about saving your liver.
Research shows that when overweight people with NAFLD lose 5-7% of body weight, their liver fat decreases by roughly 50%. Imaging shows clear improvement.
Losing more than that (10%+) can actually reverse NASH and reduce scarring.
How to Do It:
- Eat 300-500 fewer calories daily than you burn (not extreme)
- Focus on protein and fiber (they keep you full)
- Move more (see exercise section)
- Lose steadily—1-2 pounds weekly is sustainable
Realistic Timeline: 6-8 weeks to see imaging improvements, 12 weeks for enzyme changes.
Exercise Guidelines
You don’t need to become a gym rat. Moderate movement works just as well as intense exercise for liver health.
Weekly Target: 150 minutes of moderate activity (you can talk but not sing) or 75 minutes of vigorous activity (hard to talk).
What Counts:
- Brisk walking
- Swimming
- Cycling
- Dancing
- Jogging
- Team sports
Resistance Training: 2 days weekly doing weights or bodyweight exercises. This builds muscle, which helps your liver metabolize fat better.
Real Talk: Start with what you’ll actually do. A 20-minute daily walk beats a gym membership you never use.
Sleep and Stress
Your liver regenerates most during sleep. Poor sleep worsens liver disease and makes weight loss harder.
Sleep Goals:
- 7-9 hours nightly
- Consistent bedtime and wake time
- Dark, cool bedroom
- No screens 30 minutes before bed
Stress Matters: Chronic stress increases inflammation throughout your body, including your liver. Find what works for you—meditation, yoga, time in nature, therapy, or hobbies.
Even 10 minutes daily of deep breathing helps.
Simple Liver-Friendly Recipes
Recipe 1: Omega-3 Baked Salmon with Roasted Vegetables
Why This Helps: Salmon provides EPA and DHA (omega-3s that reduce liver fat). Vegetables add fiber and antioxidants.
Ingredients (Serves 2):
- 2 salmon fillets (4 oz each)
- 2 cups broccoli florets
- 1 medium bell pepper, chopped
- 1 medium zucchini, sliced
- 2 tablespoons olive oil
- 1 lemon, sliced
- 2 cloves garlic, minced
- Sea salt and black pepper
- Fresh herbs (dill or parsley)
Instructions:
Preheat oven to 400°F. Line a baking sheet with parchment paper.
Toss vegetables with 1 tablespoon olive oil, garlic, salt, and pepper. Spread on half the baking sheet.
Place salmon on the other half. Drizzle with remaining olive oil. Season with salt, pepper, and herbs. Top with lemon slices.
Bake 15-18 minutes until salmon flakes easily and vegetables are tender.
Prep Time: 10 minutes | Cook Time: 18 minutes | Cost: $6-8 per serving
Nutrition Highlights: 30g protein, 2,000+ mg omega-3s, 5g fiber
Recipe 2: Mediterranean Chickpea Salad
Why This Helps: Chickpeas provide plant protein and soluble fiber. Olive oil offers anti-inflammatory compounds.
Ingredients (Serves 4):
- 2 cans chickpeas (15 oz each), drained and rinsed
- 1 cucumber, diced
- 1 cup cherry tomatoes, halved
- 1 red bell pepper, diced
- 1/2 red onion, finely minced
- 1/4 cup fresh parsley, chopped
- 2 tablespoons fresh lemon juice
- 3 tablespoons extra-virgin olive oil
- 2 cloves garlic, minced
- Salt and pepper to taste
Instructions:
Add chickpeas, cucumber, tomatoes, bell pepper, and onion to a large bowl.
In a small bowl, whisk together lemon juice, olive oil, garlic, salt, and pepper.
Pour dressing over vegetables and chickpeas. Toss gently but thoroughly.
Add fresh parsley and stir. Chill at least 30 minutes before serving.
Prep Time: 15 minutes | Chill Time: 30 minutes | Cost: $2-3 per serving
Nutrition Highlights: 12g protein, 10g fiber, 2,000+ mg polyphenols
Make-Ahead Tip: Store in the fridge 3-4 days. Great for meal prep.
Recipe 3: Turmeric Lentil Soup
Why This Helps: Turmeric contains curcumin (anti-inflammatory). Lentils provide protein and fiber. Garlic and ginger add antioxidants.
Ingredients (Serves 6):
- 1 cup dry lentils, rinsed
- 6 cups low-sodium vegetable broth
- 1 can diced tomatoes (14.5 oz)
- 1 medium onion, diced
- 3 cloves garlic, minced
- 1 tablespoon fresh ginger, minced
- 2 teaspoons turmeric powder
- 1 teaspoon cumin
- 2 tablespoons olive oil
- 1 cup spinach
- Sea salt and pepper
- Juice of 1 lemon
Instructions:
Heat olive oil in a large pot over medium heat. Add onion and cook 5 minutes until soft. Add garlic and ginger, cook 1 minute more.
Add turmeric and cumin. Stir for 30 seconds until fragrant.
Add lentils, broth, and tomatoes. Bring to a boil, then reduce heat to simmer.
Cook 25-30 minutes until lentils are tender but not mushy.
Stir in spinach and lemon juice. Cook 2 more minutes until spinach wilts.
Season with salt and pepper to taste.
Prep Time: 10 minutes | Cook Time: 35 minutes | Cost: $1.50-2 per serving
Nutrition Highlights: 18g protein, 15g fiber, 250+ mg curcumin
Freezer Friendly: Makes great leftovers. Freeze up to 3 months.
Recipe 4: Green Tea and Walnut Smoothie
Why This Helps: Green tea provides antioxidants (but in safe amounts from a beverage). Walnuts have omega-3s. Berries add fiber and polyphenols.
Ingredients (Serves 2):
- 1 cup brewed green tea, cooled to room temperature
- 1 frozen banana
- 1 cup frozen blueberries
- 1/4 cup plain Greek yogurt (or dairy-free alternative)
- 1/4 cup raw walnuts
- 1 tablespoon raw honey
- 1/2 teaspoon vanilla extract
- Pinch of cinnamon
Instructions:
Brew green tea and let cool completely before blending (heat damages some nutrients).
Add tea, banana, blueberries, yogurt, walnuts, honey, vanilla, and cinnamon to a blender.
Blend on high for 60-90 seconds until smooth.
Pour into glasses and serve immediately.
Prep Time: 5 minutes | Cost: $2-3 per serving
Nutrition Highlights: 8g protein, 5g fiber, 500+ mg polyphenols
Storage: Best consumed fresh, but keeps 24 hours in the fridge.
Supplement Quality Matters: What to Look For
Not all supplements are created equal. The supplement industry has minimal regulation compared to medications. Here’s what separates quality from garbage.
Third-Party Testing
Real quality brands send their products to independent labs for testing. Look for these certifications:
NSF Certified: NSF tests for purity, label accuracy, and contaminants. If it says NSF on the bottle, it’s been verified.
USP Verified: U.S. Pharmacopeia tests ingredients and manufacturing. Very rigorous standard.
ConsumerLab Approved: Third-party tests for quality and accuracy. Their website lists tested products.
If It Says None of These: Be skeptical. The company might not care about quality.
Read the Label Carefully
Active Ingredient Percentage: If buying curcumin, the label should say “80% curcuminoids” or similar. Without this, you’re getting fillers.
Bioavailability Enhancements: For curcumin, look for “phytosomal” or “with piperine.” These increase absorption dramatically.
Proprietary Blends: Avoid bottles listing “liver support blend 500 mg” without breaking down individual ingredients. You don’t know how much of each you’re getting.
Unnecessary Fillers: Microcrystalline cellulose is fine. But if the ingredient list is longer than the active ingredients, question why.
Brand Reputation
Research the company. Do independent reviews exist? What do customers say on non-affiliate sites? How long have they been in business?
New brands aren’t necessarily bad, but established companies with good reviews are safer bets.
Cost vs. Quality
Cheap supplements sometimes work fine. But the cheapest option usually means cut corners somewhere—less active ingredient, poor absorption, or less rigorous testing.
Mid-range is often the sweet spot. You’re paying for quality without unnecessary markup.
Storage Matters
Some supplements degrade quickly. Keep them cool and dry. Bathroom moisture damages them. A bedroom closet is better than a bathroom cabinet.
Check expiration dates. Old supplements lose potency or can develop contaminants.
Red Flags: When to See Your Doctor Immediately
Stop taking supplements and contact your doctor right away if you experience:
Jaundice (yellowing of skin and eyes): This means bilirubin is building up. Your liver isn’t processing it properly. Serious warning sign.
Dark urine or pale stools: Your liver isn’t producing bile properly or isn’t moving it. Needs immediate evaluation.
Severe abdominal pain: Could indicate liver inflammation or other serious conditions.
Unexplained bruising or bleeding: Your liver makes clotting factors. Easy bruising suggests liver failure starting.
Extreme fatigue or confusion: Liver disease can cause encephalopathy (brain fog from toxin buildup). Requires urgent care.
Swelling in legs or belly: Sign of liver failure with fluid buildup.
Fever with abdominal pain: Possible infection or acute liver inflammation.
Don’t assume supplements caused these. Many things can cause them. But see your doctor immediately to rule out serious problems.
Timeline for Results: What to Expect
Different supplements work on different timelines. Understanding this prevents you from quitting too early or expecting instant miracles.
| Supplement | Enzyme Improvements | Imaging Changes | Symptom Relief | Your Action |
|---|---|---|---|---|
| Vitamin E (NASH) | 8-12 weeks | 16-24 weeks | 12+ weeks | Requires medical monitoring |
| NAC | 4-8 weeks | N/A usually | 2-4 weeks (energy) | Consistent daily use |
| SAMe | 6-12 weeks | 8-16 weeks | 8-12 weeks | Check in with doctor |
| Milk Thistle | 6-12 weeks | Not usually tracked | 8-12 weeks | Stay consistent |
| Omega-3 | 8-12 weeks | 12-16 weeks | 4-8 weeks | Take with food |
| Curcumin | 8-12 weeks | 12-16 weeks | 6-10 weeks | Use bioavailable form |
| Choline | 8-12 weeks | 12-16 weeks | Varies | Dietary sources first |
| Artichoke | 8-12 weeks | 12-16 weeks | 8-12 weeks | Mild benefits expected |
| Lifestyle (diet + exercise) | 4-8 weeks | 8-12 weeks | 2-4 weeks | Biggest impact overall |
| Weight loss (5-7%) | 6-12 weeks | 8-16 weeks | 2-4 weeks | Life-changing for fatty liver |
General Rule: Give any supplement 12 weeks before deciding if it works. Your body needs time to respond.
Blood Work Timeline: Get baseline liver tests before starting. Retest at 12 weeks. Then every 6 months if doing well.
Imaging Timeline: Ultrasounds typically happen yearly. Fibroscan can be done more frequently. Ask your doctor.
Your Actionable Strategy for Liver Health
Rule 1: Doctor First
No article replaces your own doctor’s advice based on your complete health history. They know your medications, your conditions, and your risks. We don’t.
Have a specific conversation: “I want to support my liver health with supplements. What do you recommend for my situation?” Let them guide you.
Rule 2: Focus on the Tiers
Tier 1 & 2 Supplements: These have solid evidence. If they match your condition and your doctor approves, they’re worth trying.
Tier 3 Supplements: Emerging evidence. Use them only under doctor guidance. They might help, but proof is still developing.
Tier 4 Supplements: Skip most of these unless you’re deficient in that nutrient. Marketing hype outweighs evidence here.
Rule 3: Start Simple, Not Overwhelming
Don’t take 10 supplements at once. Pick 2-3 that match your situation. Take them consistently for 12 weeks. Then assess.
More isn’t better. Better is better.
Rule 4: Lifestyle Is Still King
Supplements are helpers. They’re not magic bullets. A healthy diet, regular movement, and healthy weight are the real foundation of liver health.
No supplement beats:
- Losing 5-7% of body weight
- Moving 150 minutes weekly
- Eating mostly whole foods
- Limiting alcohol
- Managing stress and sleep
Do these first. Add supplements as support.
Rule 5: Track Your Progress
Keep simple notes:
- What supplements you’re taking
- Your doses
- Any symptoms or changes
- Your energy level
- Your digestion
Share this with your doctor at each visit. Evidence matters more than feelings, but your experience counts.
Rule 6: Get Tested, Don’t Guess
Don’t assume your liver is fine because you feel okay. People with serious liver disease often feel fine until it’s advanced.
Get baseline tests. Retest as recommended. Imaging helps too. Numbers don’t lie.
Rule 7: Be Patient and Realistic
Your liver didn’t get damaged overnight. It won’t heal overnight either. Consistent effort over months shows results. Sporadic effort shows nothing.
Take your supplements daily. Stick with lifestyle changes. Give it time. Expect modest, steady improvements rather than dramatic turnarounds.
Conclusion
Your liver does incredible work every single day. It deserves real care, not just marketing hype.
You now have evidence-based information to make informed decisions. You know which supplements have strong proof and which are just wishful thinking. You understand your condition better. You know what tests matter and what timelines to expect.
Here’s what to do next:
Step 1: Schedule a doctor visit. Bring this guide. Discuss your liver health and supplement options.
Step 2: Get baseline blood work and imaging if you haven’t recently.
Step 3: Based on your condition and doctor’s guidance, choose 2-3 supplements from Tier 1 or 2.
Step 4: Focus hard on lifestyle—diet, movement, sleep, and stress management. This is where the real healing happens.
Step 5: Give it 12 weeks. Retest. Adjust based on results.
FAQs
Can I Take Multiple Supplements Together?
Yes, most combinations are safe. But too many at once can cause stomach upset.
Smart Approach: Start with one supplement. After 2 weeks, add a second if needed. This helps you spot which one causes any issues.
Watch for Interactions: Some supplements compete for absorption. For example, iron and calcium fight for absorption. Take them 2 hours apart.
Ask Your Pharmacist: Many interactions happen with medications, not other supplements. Your pharmacist has access to interaction databases.
When Should I Stop a Supplement?
Stop if you experience:
- Severe abdominal pain or nausea lasting more than a few hours
- Yellowing of skin or eyes (jaundice)
- Unexplained bruising or bleeding
- Dark urine or pale stools
- Severe headache or dizziness
- Allergic reactions (rash, swelling, difficulty breathing)
Minor Issues: Mild nausea, upset stomach, or headache might mean you need food with it or a lower dose. Try that first before quitting.
Will Supplements Replace My Liver Medication?
No. Never stop prescribed medications to take supplements instead. Supplements are additions to medical treatment, not replacements.
Your doctor prescribed medication for a reason. Supplements support that treatment but don’t have the same power.
Is It Safe During Pregnancy?
Most supplements haven’t been tested in pregnant people. Talk to your obstetrician before taking anything. Some supplements carry risks to developing babies.
NAC, milk thistle, and omega-3s are generally considered safe during pregnancy, but confirm with your doctor first.
What About Alcohol Use?
Alcohol damages your liver regardless of supplements. If you have liver disease, your doctor likely wants you to stop completely.
If you don’t have liver disease but drink regularly, know that supplements won’t protect you from alcohol damage. Cutting back or stopping is what actually helps.


