If you’re dealing with numbness, pain, or weakness that seems to radiate from your elbow down to your hand, you might have ulnar nerve entrapment, also known as cubital tunnel syndrome.
This complete guide will walk you through targeted exercises that can help ease your symptoms and get you back to normal activities. But first, let’s make sure you’re in the right place and understand exactly what you’re dealing with.
Understanding your ulnar nerve: the complete picture
What is ulnar nerve entrapment (cubital tunnel syndrome)?
Think of your ulnar nerve as a telephone wire running from your neck to your hand. When this nerve gets squeezed or compressed—usually at the elbow—it can’t send signals properly. This creates the numbness, tingling, and pain you’re feeling.
The ulnar nerve is the second most commonly compressed nerve in your body, affecting up to 6% of adults at some point in their lives. It controls sensation in your ring and pinky fingers and powers many of the small muscles in your hand that help with grip strength and fine motor tasks.
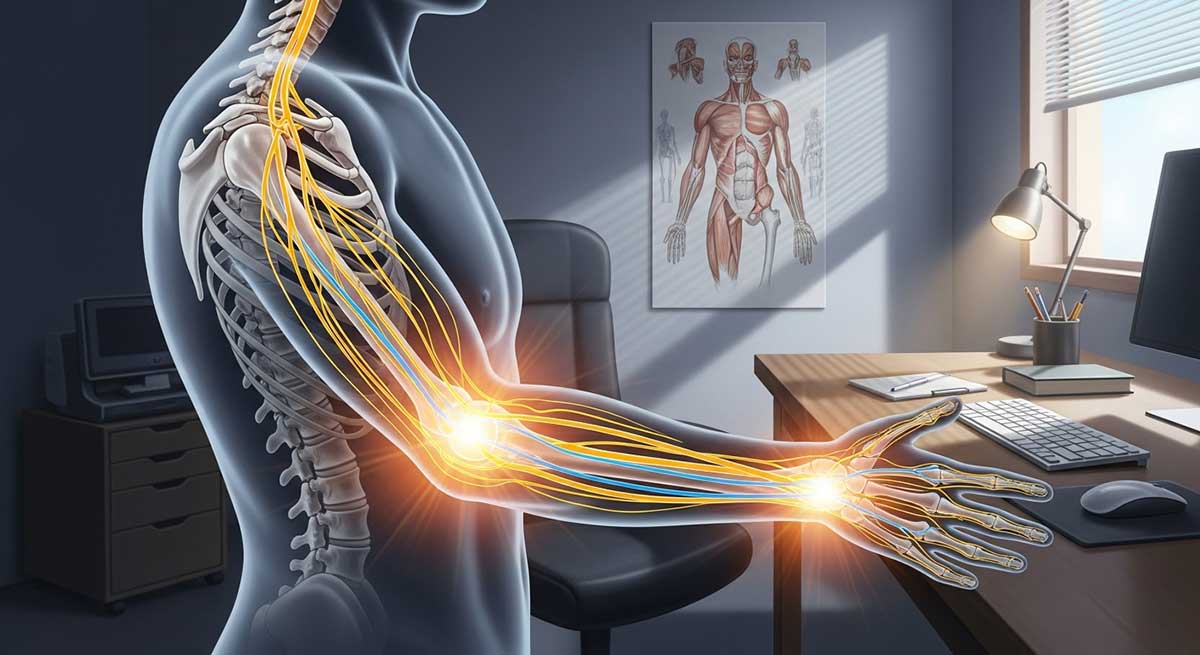
Your ulnar nerve pathway: where problems happen
Understanding where your nerve travels helps you understand why certain positions make symptoms worse.
| Location | Anatomical structure | Common causes | Symptoms |
|---|---|---|---|
| Cubital Tunnel (Elbow) | Medial epicondyle groove | Prolonged elbow bending, sleeping with bent elbow, leaning on elbow | Ring/pinky numbness, elbow pain, weakness |
| Guyon’s Canal (Wrist) | Between pisiform and hamate bones | Cycling, prolonged wrist pressure, repetitive gripping | Hand weakness, no forearm symptoms |
| Thoracic Outlet | First rib/clavicle area | Poor posture, neck positioning, overhead activities | Whole arm symptoms, shoulder pain |
The elbow location (cubital tunnel) accounts for about 85% of all ulnar nerve compression cases.
Assess your risk factors
Understanding your personal risk helps you make better decisions about treatment and prevention.
| Risk category | Specific factors | Your risk level |
|---|---|---|
| Occupational | Computer work >6 hours/day, assembly line work, musicians, carpenters, plumbers | Check all that apply |
| Medical conditions | Diabetes, rheumatoid arthritis, thyroid disorders, previous elbow fractures | Rate: High/Medium/Low |
| Lifestyle factors | Sleep on stomach with arms under pillow, frequent phone use, prolonged driving | Count your risk factors |
| Physical factors | BMI >30, pregnancy, fluid retention, joint hypermobility | Assess current status |
Scoring: 0-2 factors = Low risk, 3-5 factors = Moderate risk, 6+ factors = High risk
Are you in the right place? Advanced self-assessment
Ulnar nerve entrapment severity scale
Before starting exercises, understand where you fall on the severity spectrum:
| Severity level | Symptoms | Daily impact | Exercise approach | Medical need |
|---|---|---|---|---|
| Mild | Occasional tingling, symptoms only with certain positions | Minimal disruption to daily tasks | Focus on nerve gliding and prevention | Monitor symptoms |
| Moderate | Persistent numbness, mild grip weakness, night symptoms | Some activity limitations, sleep disruption | Add strengthening, consider splinting | Consider professional evaluation |
| Severe | Constant symptoms, obvious muscle weakness, dropping objects | Significant functional loss, work impact | Medical evaluation essential before exercises | Urgent professional care needed |
Is it really ulnar nerve entrapment?
Many conditions can mimic ulnar nerve problems. This comparison helps you understand the differences:
| Condition | Similar symptoms | Key differences | Simple test |
|---|---|---|---|
| Carpal Tunnel Syndrome | Hand numbness and tingling | Affects thumb, index, middle fingers | Make “prayer” position – worsens carpal tunnel symptoms |
| Cervical Radiculopathy | Arm pain and numbness | Neck pain, affects multiple fingers | Turn head away from affected side – may worsen symptoms |
| Thoracic Outlet Syndrome | Upper limb tingling | Affects whole arm, worse overhead | Raise both arms overhead for 3 minutes – reproduces symptoms |
| Tennis Elbow | Elbow pain | No numbness, pain on outside of elbow | Resist wrist extension – causes pain in tennis elbow |
Quick self-assessment tests
Test 1: Elbow flexion test
- Sit with your affected arm at your side
- Bend your elbow fully and hold for 60 seconds
- Note any increase in numbness or tingling
Test 2: Tinel’s sign
- Gently tap the inside of your elbow where you feel your “funny bone”
- If this creates tingling down to your ring and pinky fingers, it suggests ulnar nerve irritation
Important: These tests are for information only. Always get a proper medical diagnosis before starting any treatment program.
Before you start: essential safety and evidence-based guidelines
The science behind exercise for nerve entrapment
Research shows that specific exercises can improve nerve gliding, reduce inflammation, and strengthen supporting muscles. Studies report 60-80% success rates with conservative exercise programs when started early and performed consistently.
What you should feel vs. warning signs
Normal exercise sensations:
- Mild pulling or stretching feeling
- Slight muscle tension
- Gradual warming of the area
- Temporary mild achiness after exercise
Stop immediately if you experience:
- Sharp, shooting pain
- Increased numbness or tingling during or after exercise
- Electrical sensations
- Complete loss of feeling
- Severe weakness that affects daily tasks
Red flag symptoms: when to seek immediate medical care
| Symptom | Urgency level | Possible cause | Action required |
|---|---|---|---|
| Complete numbness in ring/pinky fingers | Emergency | Severe nerve compression | Emergency room or urgent care |
| Sudden onset of significant weakness | Urgent | Acute nerve injury | Same-day medical appointment |
| Symptoms spreading to other fingers | Semi-urgent | Progressive nerve damage | Medical evaluation within 1-2 days |
| Muscle wasting in hand | Urgent | Advanced nerve damage | Immediate specialist referral |
Exercise frequency and dosage guidelines
Phase-based approach:
- Acute Phase (0-2 weeks): 3 times daily, very gentle movements
- Recovery Phase (2-8 weeks): 2 times daily, full range exercises
- Maintenance Phase (8+ weeks): 1 time daily, strength focus
Your personalized exercise prescription
Instead of one-size-fits-all exercises, here’s your personalized approach based on symptoms and goals:
| Exercise type | Acute phase (weeks 0-2) | Recovery phase (weeks 2-8) | Maintenance phase (8+ weeks) |
|---|---|---|---|
| Nerve Gliding | 3x daily, gentle range of motion | 2x daily, full range of motion | 1x daily, preventive maintenance |
| Stretching | Avoid if painful | Hold 30 seconds, 3 repetitions | Hold 45 seconds, 2 repetitions |
| Strengthening | None recommended | Light resistance, focus on form | Progressive resistance training |
| Frequency | As tolerated, stop if symptoms worsen | Daily consistency | 3-4 times weekly |
Phase 1: Calming the nerve – advanced gliding techniques
Nerve gliding exercises help your compressed ulnar nerve move freely through surrounding tissues. Think of it as physical therapy for your nerve.
Exercise 1: Progressive ulnar nerve glide
Beginner version:
- Sit with your arm at your side, elbow straight
- Raise your arm out to the side at shoulder height
- Bend your elbow to 90 degrees, palm facing down
- Slowly turn your palm up toward the ceiling
- Hold for 15 seconds, return to start
Advanced version:
- Follow steps 1-4 above
- Gently bend your wrist back, fingers pointing down
- Tilt your head away from your raised arm
- Hold for 30 seconds, feeling gentle stretch from neck to fingers
Exercise 2: Dynamic head tilt nerve mobilization
Starting position:
Sit tall, both arms at sides
Movement pattern:
- Tilt head toward unaffected side
- Raise affected arm out to side
- Bend elbow, place hand behind head
- Gently increase head tilt with opposite hand
- Hold 20 seconds, then reverse movement slowly
- Repeat 5-10 times in flowing motion
Exercise 3: “Nerve flossing” technique
This advanced technique helps the nerve glide through tight areas:
- Start with affected arm at side
- Make “OK” sign with thumb and index finger
- Place circle over eye like a mask
- Tilt head toward same shoulder
- Slowly straighten elbow while maintaining “mask”
- Return to start position
- Repeat 15-20 times in smooth, rhythmic motion
Progression tips:
- Week 1-2: Slow, gentle movements
- Week 3-4: Increase range of motion
- Week 5+: Add slight overpressure at end range
Phase 2: Flexibility revolution – strategic muscle releases
Tight muscles around your elbow and wrist create extra pressure on your ulnar nerve. These targeted stretches create space for nerve healing.
Exercise 4: Advanced wrist flexor release
Basic stretch:
- Extend affected arm, palm up
- Use other hand to pull fingers back gently
- Hold 30 seconds, feel stretch along inner forearm
Advanced variation:
- Perform basic stretch
- Add gentle side-to-side finger movement
- Include slight elbow extension for deeper stretch
- Hold positions for 45 seconds each
Exercise 5: Comprehensive wrist extensor stretch
Step-by-step:
- Extend arm straight ahead, palm down
- Make loose fist
- Use other hand to push fist down and toward body
- Keep elbow completely straight
- Hold 30 seconds, breathe deeply
Modification for severe cases:
- Support arm on table
- Use very gentle pressure
- Hold for shorter periods (15 seconds)
Exercise 6: Neck and shoulder tension release
Complete sequence:
- Shoulder Rolls: 10 backward, 10 forward
- Neck Side Bends: Hold each side 15 seconds
- Gentle Rotations: 5 each direction (avoid forcing)
- Upper Trap Stretch: Pull head to side, hold 30 seconds each
Phase 3: Building resilient support – strength training protocol
Strong, stable muscles provide better joint support and reduce future nerve compression risk.
Exercise 7: Progressive grip strengthening
Equipment needed:
Stress ball, putty, or rolled towel
Beginner protocol:
- Light squeeze, 5 seconds hold
- 10 repetitions, 3 times daily
- Progress weekly by adding 1-2 repetitions
Intermediate protocol:
- Medium resistance, 8 seconds hold
- 15 repetitions, 2 times daily
- Add finger extension exercises
Advanced protocol:
- Firm resistance, 10 seconds hold
- 20 repetitions, daily
- Include finger isolation exercises
Exercise 8: Functional wrist strengthening
Equipment:
1-3 pound weight or soup can
Wrist flexion (palm up):
- Rest forearm on table, hand over edge
- Hold weight, slowly curl wrist up
- Lower with control
- Start: 10 reps, Progress to: 20 reps
Wrist extension (palm down):
- Flip hand over, palm down
- Lift wrist against weight
- Lower slowly
- Same progression as flexion
Weekly progression schedule:
- Week 1-2: Body weight only
- Week 3-4: 1 pound weight
- Week 5-6: 2 pound weight
- Week 7+: 3 pounds or resistance band
Exercise 9: Advanced forearm rotation training
Equipment:
Light hammer or weighted object
Technique:
- Rest forearm on table, hand hanging over
- Hold hammer by handle, weight pointing up
- Rotate forearm to move weight like windshield wiper
- Complete range: palm up to palm down
- 15 repetitions each direction
Progression markers:
- Can complete without pain
- Full range of motion achieved
- No increase in symptoms after exercise
Beyond exercises: your complete prevention strategy
Workplace ergonomic optimization
| Work area | Optimal setup | Common mistakes | Evidence-based solutions |
|---|---|---|---|
| Desk Height | Elbows at 90° when typing | Desk too high (>90°) or low (<90°) | Adjustable desk or keyboard tray |
| Armrest Position | Support forearms, not elbows | Direct pressure on elbow nerve | Pad armrests, adjust height |
| Keyboard/Mouse | Neutral wrist, light touch | Extended or flexed wrists | Ergonomic keyboard, mouse pad with wrist support |
| Phone Use | Headset or hands-free | Cradling phone with shoulder | Bluetooth headset, speakerphone |
| Break Schedule | 5 minutes every 30 minutes | Continuous work >2 hours | Set automatic reminders |
Sleep position modifications
Problem positions that worsen symptoms:
- Sleeping with arm under pillow
- Side sleeping with bent elbow
- Stomach sleeping with arms folded
Optimal sleep setup:
- Back Sleepers: Arms at sides, pillow under forearms
- Side Sleepers: Body pillow between arms, straight elbow
- Universal: Towel wrap around elbow to prevent bending
Activity-specific prevention strategies
| Activity level | Daily prevention routine | Weekly maintenance | Monthly assessment |
|---|---|---|---|
| Sedentary Worker | 5-minute stretch breaks every hour | 3 strengthening sessions | Workstation ergonomic review |
| Active/Athletic | Pre-activity nerve warmup | Sport-specific conditioning | Performance and symptom tracking |
| Manual Laborer | Job rotation, proper tool grip | Strength and flexibility focus | Ergonomic technique review |
Your recovery roadmap: what to expect
Evidence-based recovery timeline
| Time period | Expected improvements | Warning signs | Recommended actions |
|---|---|---|---|
| Week 1-2 | Reduced acute pain, better sleep | Worsening numbness, increased weakness | Modify activities, consider splinting |
| Week 3-4 | Improved comfort during daily tasks | No pain reduction, persistent night symptoms | Add gentle strengthening, ergonomic review |
| Week 5-8 | Better grip strength, reduced tingling | Muscle wasting, dropping objects | Consider physical therapy evaluation |
| Week 9-12 | Return to normal activities | Persistent significant symptoms | Specialist referral, advanced imaging |
Progress tracking sheet
Use this table to monitor your improvement:
| Week | Pain level (0-10) | Numbness (0-10) | Grip strength (Weak/Fair/Good) | Functional tasks (List 3) | Exercise tolerance | Notes |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| Week 2 | ||||||
| Week 4 | ||||||
| Week 6 | ||||||
| Week 8 | ||||||
| Week 12 |
Success indicators
You’re on the right track if:
- Pain decreases by 2-3 points on 10-point scale
- Numbness episodes become less frequent
- Sleep quality improves
- Daily tasks become easier
- Exercise tolerance increases
When exercises aren’t enough: professional treatment options
Comprehensive treatment comparison
| Treatment option | Success rate | Recovery time | Ideal candidates | Potential risks | Cost range |
|---|---|---|---|---|---|
| Conservative Exercise | 60-80% | 6-12 weeks | Mild to moderate symptoms | Minimal | Low |
| Night Splinting | 40-70% | 4-8 weeks | Night symptoms prominent | Skin irritation | Low-moderate |
| Physical Therapy | 70-85% | 8-16 weeks | Moderate cases, poor technique | Minimal | Moderate |
| Corticosteroid Injection | 50-70% | 2-6 weeks | Acute inflammation | Temporary weakness | Moderate |
| Nerve Decompression Surgery | 85-95% | 3-6 months | Severe cases, failed conservative care | Surgical complications | High |
Making the right treatment decision
Choose conservative exercise if:
- Symptoms present <6 months
- Mild to moderate severity
- No muscle wasting
- Motivated for daily exercise
Consider professional help if:
- No improvement after 6-8 weeks
- Moderate to severe symptoms
- Work or daily activities significantly affected
- Unclear diagnosis
Exercise troubleshooting guide
| Problem | Possible cause | Solution | When to stop |
|---|---|---|---|
| Increased tingling during exercise | Exercise too aggressive | Reduce intensity by 50% | If symptoms persist >24 hours |
| No improvement after 4 weeks | Wrong technique or diagnosis | Video record exercises, seek evaluation | Consider alternative treatments |
| Morning stiffness and pain | Poor sleep positioning | Sleep modifications, night splint | If affecting work performance |
| Weakness getting worse | Overexercise or progression | Return to earlier phase exercises | If dropping objects frequently |
| Symptoms spreading to other fingers | Possible multiple nerve involvement | Stop exercises, seek medical evaluation | Immediately |
Advanced topics: special considerations
Technology integration for better outcomes
Helpful apps and tools:
- Exercise reminder apps (set for every 2 hours)
- Ergonomic assessment apps for workstation setup
- Symptom tracking apps for progress monitoring
- Telemedicine platforms for follow-up care
Special population guidelines
Pregnant women:
- Higher risk due to fluid retention
- Focus on gentle exercises only
- Avoid prolonged static positions
- Consider professional monitoring
Athletes and musicians:
- Sport/instrument-specific modifications
- Emphasis on prevention strategies
- May need activity modification during healing
- Consider performance impact of treatments
Older adults:
- Start more gradually
- Consider comorbid conditions (diabetes, arthritis)
- May need longer recovery time
- Higher risk of surgical complications
Your action plan: getting started today
Week 1-2: Foundation phase
Daily tasks:
- Complete self-assessment and severity rating
- Begin Phase 1 nerve gliding exercises
- Implement basic ergonomic changes
- Start progress tracking
Goals:
- Establish exercise routine
- Identify main symptom triggers
- Begin symptom improvement
Week 3-4: Building phase
Daily tasks:
- Continue nerve gliding, add gentle stretching
- Optimize sleep position
- Refine workplace ergonomics
- Monitor progress weekly
Goals:
- Increase exercise tolerance
- Reduce night symptoms
- Improve daily function
Week 5-8: Strengthening phase
Daily tasks:
- Add strengthening exercises
- Focus on prevention strategies
- Consider professional evaluation if needed
- Track functional improvements
Goals:
- Build supporting muscle strength
- Achieve consistent symptom relief
- Return to normal activities
Week 9-12: Maintenance phase
Daily tasks:
- Maintain exercise routine
- Continue ergonomic practices
- Monitor for symptom recurrence
- Plan long-term prevention
Goals:
- Prevent symptom return
- Optimize long-term function
- Develop lifelong healthy habits
Conclusion
This comprehensive guide provides evidence-based information and exercises that have helped thousands of people with ulnar nerve entrapment. However, everyone’s situation is unique. Always consult with a healthcare professional for proper diagnosis and personalized treatment recommendations.
Your ulnar nerve entrapment doesn’t have to control your life. With the right knowledge, consistent effort, and appropriate professional guidance when needed, most people can achieve significant relief and return to their normal activities. Stay patient with the process, be consistent with your exercises, and don’t hesitate to seek help when you need it.
FAQs
Can these exercises make symptoms worse?
When performed correctly, these exercises should help. However, 10-15% of people may experience temporary symptom increase during the first week. This usually indicates:
- Exercise intensity too high initially
- Nerve is very irritated and needs gentler approach
- Possible incorrect diagnosis
What to do: Reduce exercise intensity by 50% and continue. If symptoms worsen after one week, stop and seek professional evaluation.
How long until I feel relief?
Research shows:
- 30% notice improvement within 2 weeks
- 60% see significant improvement by 6 weeks
- 80% reach maximum benefit by 12 weeks
Factors affecting recovery speed:
- Symptom duration before starting treatment
- Severity of compression
- Consistency with exercise program
- Ergonomic modifications
- Overall health status
Should I use ice or heat?
Evidence-based recommendations:
Use Ice When:
- Acute pain or swelling after exercise
- Sharp, shooting pains
- First 48 hours of symptom flare-up
- Apply for 15-20 minutes
Use Heat When:
- Stiffness and muscle tension
- Before exercise to warm tissues
- Chronic, aching symptoms
- Apply for 15-20 minutes
Never Use Ice or Heat If:
- You have decreased sensation (may cause burns)
- Skin conditions present
- Circulation problems
Can I exercise with an elbow brace?
Depends on brace type:
- Elbow Pads: Usually safe during exercise, may actually help
- Rigid Braces: Remove during exercise, use for work/sleep
- Night Splints: Remove for exercise, crucial for sleep
General Rule: If the brace restricts movement needed for the exercise, remove it. The goal is controlled movement, not complete immobilization.
What if I have symptoms in multiple locations?
Double Crush Syndrome occurs when nerves are compressed at multiple sites. This affects 20-30% of people with ulnar nerve problems. Signs include:
- Symptoms in multiple fingers
- Neck and shoulder pain
- Worse response to single-site treatment
Recommended approach:
- Start with conservative exercises
- Address ergonomic factors comprehensively
- Seek professional evaluation if poor response
- May need targeted treatment for each compression site
Is surgery always successful?
Surgery success rates:
- Symptom relief: 85-95% see improvement
- Complete resolution: 70-80%
- Return to normal activities: 80-90%
Factors affecting success:
- Duration of symptoms before surgery
- Severity of nerve damage
- Post-surgical rehabilitation compliance
- Ergonomic modifications after surgery
Recovery timeline after surgery:
- Initial healing: 2-6 weeks
- Nerve regeneration: 3-6 months
- Maximum improvement: 12-18 months


