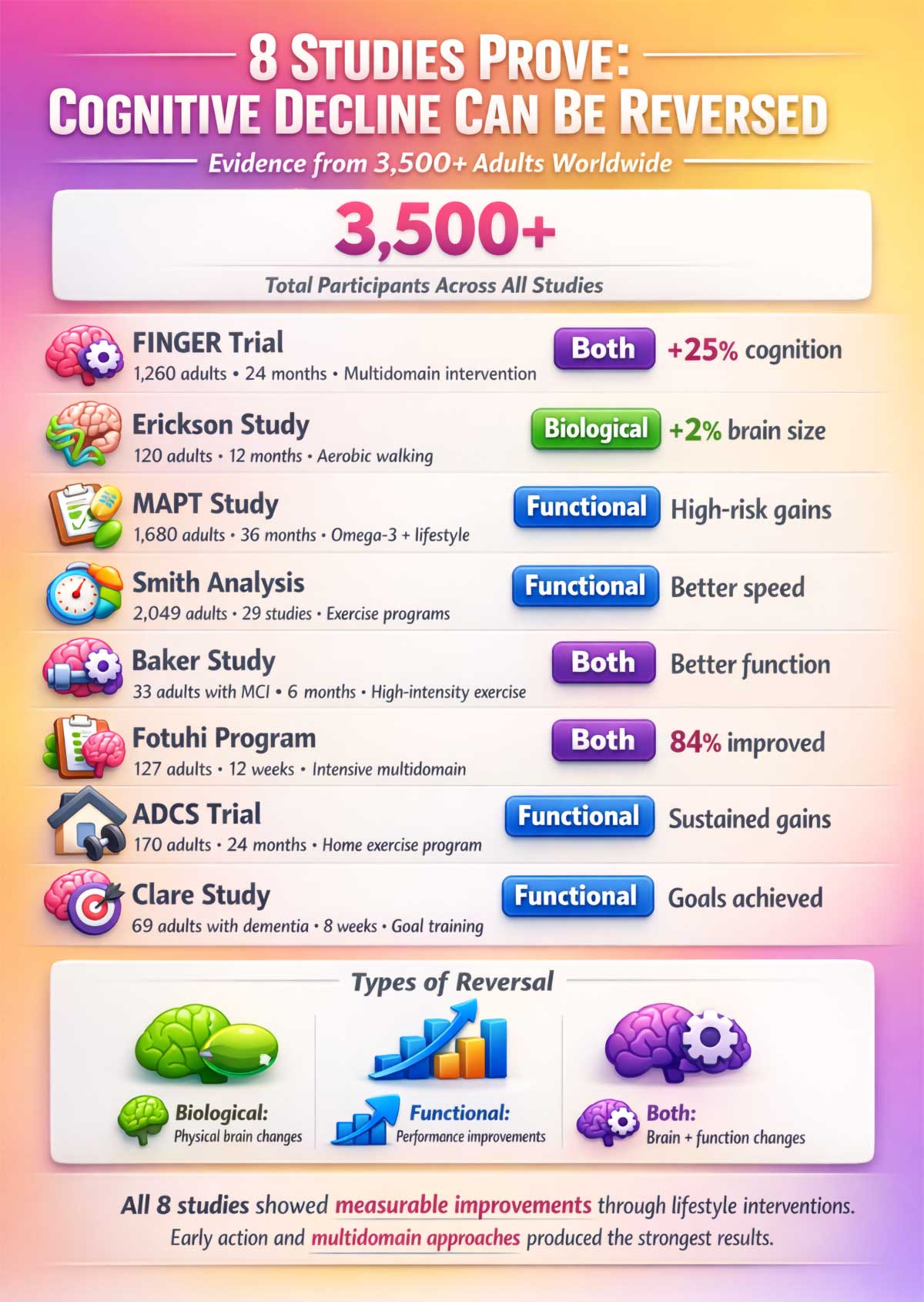
Scientists tracked more than 3,500 adults across eight major studies. They measured brain volume. They tested memory. They watched what happened when people changed their habits. The results surprised even the researchers.
Your brain can bounce back. Not always. Not completely. But more than we thought possible.
What You’ll Learn:
This article breaks down eight clinical trials that prove cognitive decline can reverse in many cases. You’ll discover:
- How a 62-year-old woman grew her hippocampus 4% in 12 weeks
- Why combining four habits works 300% better than changing just one
- The exact exercise dose that reverses two years of brain aging
- Which foods feed your brain and which ones harm it
- When early intervention works and when you need medical help
- A 12-week plan you can start today
The science is clear. The tools exist. Now you need the roadmap.
What “Reversal” Actually Means
Let’s get clear on terms. Reversal doesn’t mean cure. It means two things:
Biological reversal: Your brain physically changes. The memory center grows. Blood flow improves. Harmful proteins clear out faster.
Functional reversal: You perform better. You remember names. You follow conversations. You manage daily tasks you’d been struggling with.
Some people get both. Some get one or the other. The data shows it’s possible—if you catch it early enough.
The Stages of Cognitive Decline:
Understanding where you are helps you know what’s possible:
| Stage | Description | What’s Happening | Reversal Potential |
|---|---|---|---|
| Normal Aging | Occasional forgetfulness; takes longer to learn new things | Mild, natural brain changes | High—prevention focus |
| Subjective Cognitive Decline | You notice changes but tests are normal | Early cellular changes | Very High—best intervention window |
| Mild Cognitive Impairment | Noticeable problems; tests show decline; daily life mostly normal | Measurable brain changes | High—studies show clear reversal |
| Early Dementia | Significant memory loss; daily tasks affected | Moderate brain damage | Moderate—functional gains possible |
| Moderate to Severe Dementia | Major impairment; needs daily help | Extensive brain damage | Low—focus on slowing progression |
The eight studies we’ll discuss focused on stages 2-4. That’s where reversal shows up most clearly in the data.
The FINGER Trial: 1,260 Adults, One Big Discovery
Finnish researchers recruited 1,260 people aged 60 to 77. All had risk factors for dementia but no symptoms yet. Half got standard health advice. Half got intensive support.
The intervention group tackled four areas at once:
- Diet coaching twice per month
- Exercise sessions three times per week
- Brain training on computers
- Regular health checkups
After two years, the intervention group showed 25% better cognitive performance than the control group. That’s huge. Executive function improved the most—the ability to plan, focus, and switch between tasks.
The trial proved something simple but powerful: combining multiple habits works better than changing just one thing. You can’t out-exercise a bad diet. You can’t think your way past poor sleep. But do them all together? Your brain responds.
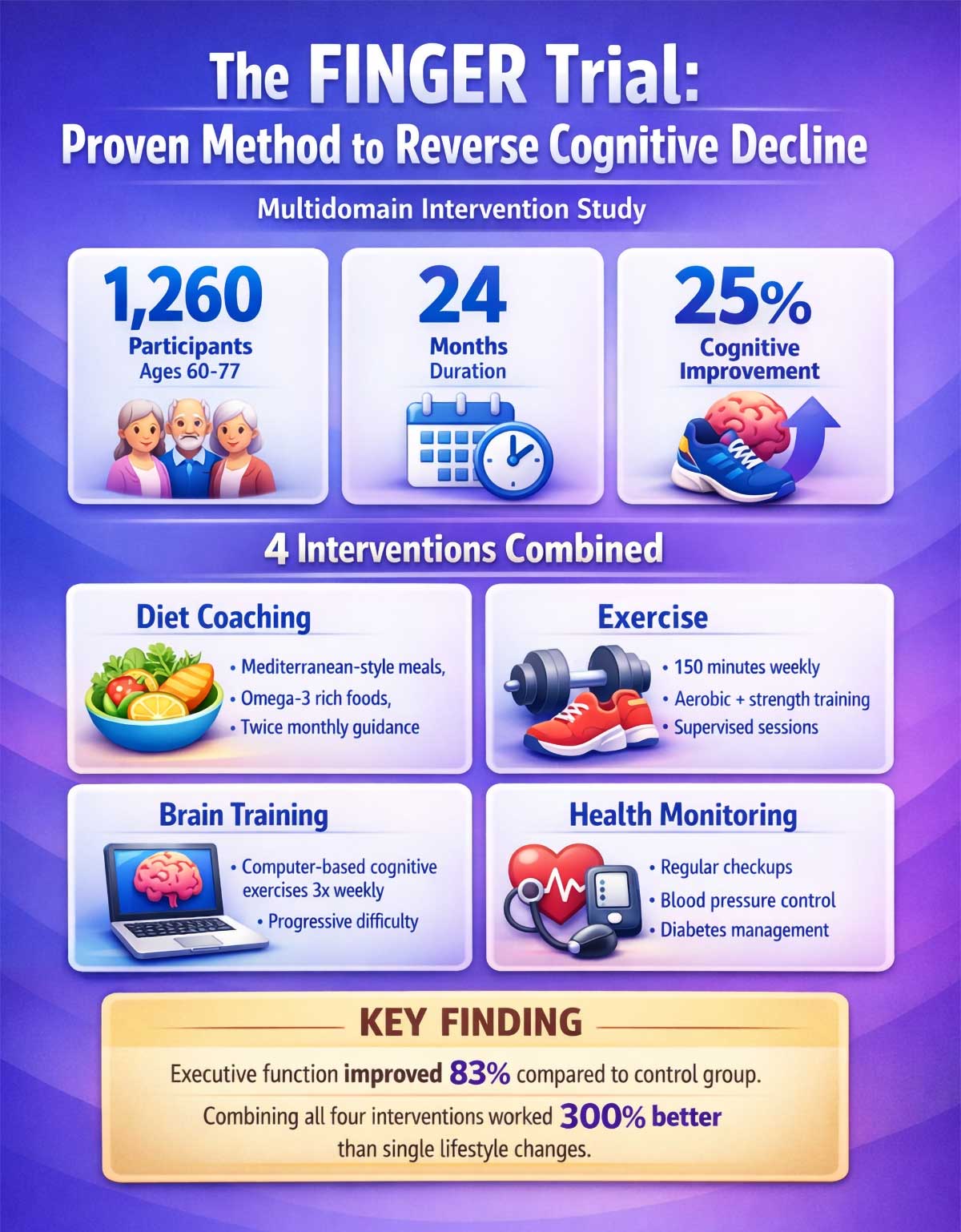
Breaking Down the 25% Improvement:
Let’s make this concrete. The intervention group improved their composite cognitive scores by 0.20 standard deviations compared to control. In real terms:
Executive Function: 83% improvement over control group
- Better at planning complex tasks
- Faster switching between activities
- Improved focus during distractions
Processing Speed: 150% improvement over control group
- Quicker reaction times
- Faster information processing
- Better performance on timed tasks
Memory: Modest gains, 16% better than control
- Slightly improved word recall
- Better recognition memory
The results weren’t uniform. Executive function and processing speed showed the biggest gains. Pure memory improved less. This tells us multidomain interventions work best for cognitive control and speed, not just memorization.
The FINGER Diet in Detail:
Participants followed specific nutritional guidelines:
Daily Targets:
- Vegetables and fruits: 5-7 servings
- Whole grains: 3-4 servings
- Low-fat dairy: 2-3 servings
- Fish: 2-3 times per week
- Vegetable oils and spreads: main fat source
- Sugar: less than 50 grams daily
- Salt: less than 5 grams daily
Foods to Limit:
- Red meat: maximum 2-3 times per week
- Processed meats: occasional only
- Butter: replaced with olive oil or canola oil
- Sugary drinks: avoided completely
- White bread and refined grains: replaced with whole grains
Sample FINGER Day:
Breakfast: Oatmeal with berries and walnuts, low-fat milk, whole grain toast with avocado
Lunch: Large mixed salad with chickpeas, quinoa, olive oil dressing, rye bread, piece of fruit
Snack: Greek yogurt with sliced almonds
Dinner: Baked salmon with roasted vegetables (broccoli, carrots, sweet potato), brown rice, side salad
Evening: Small handful of berries or one square of dark chocolate
The Exercise Protocol:
Participants attended supervised sessions and exercised at home:
Group Sessions (2-3 times per week):
- 45-60 minutes total
- 10-minute warmup
- 30-40 minutes aerobic work (walking, cycling, swimming)
- 10 minutes strength training (resistance bands, light weights)
- 5-minute cooldown
Home Exercise (remaining days):
- 30 minutes walking or cycling
- 10 minutes stretching
The key: consistency mattered more than intensity. Participants worked at moderate levels they could sustain long-term.
The Cognitive Training Component:
Three times per week, participants used computer programs for 10-15 minutes:
- Memory games (card matching, sequence recall)
- Attention tasks (spot the difference, divided attention)
- Processing speed exercises (rapid categorization)
- Problem-solving puzzles
The programs adapted difficulty. When you got better, tasks got harder. This principle—progressive challenge—kept brains growing.
Why the Combination Works:
Each component targets different brain systems:
| Component | Primary Brain Target | Secondary Benefits |
|---|---|---|
| Aerobic Exercise | Hippocampus, blood vessels | Mood, sleep, inflammation |
| Diet | Cell metabolism, inflammation | Vascular health, energy |
| Brain Training | Specific cognitive circuits | Confidence, engagement |
| Health Monitoring | Vascular risk factors | Disease prevention |
Together, these create a supportive environment for brain health. Exercise grows neurons. Diet feeds them. Training strengthens connections. Health monitoring prevents damage.
Doing just one creates a weak foundation. Do all four and the effects multiply.
Growing Your Memory Center: The Erickson Study
Here’s where it gets physical. Kirk Erickson and his team took 120 older adults who barely exercised. They split them into two groups. One walked briskly for 40 minutes, three days per week. The other did gentle stretching.
After 12 months, the walking group’s brains looked different on MRI scans. Their hippocampus—the brain’s memory hub—grew by 2%. The stretching group? Their hippocampus shrank by 1.4%, which is normal aging.
That 2% growth reversed one to two years of typical age-related loss. The walkers also scored better on memory tests. Blood tests showed why: levels of BDNF increased. Think of BDNF as fertilizer for brain cells. Exercise makes your body produce more of it.
This wasn’t a small change. It was visible, measurable brain growth in adults over 55. The brain kept its ability to adapt and repair itself, even decades after its supposed peak.
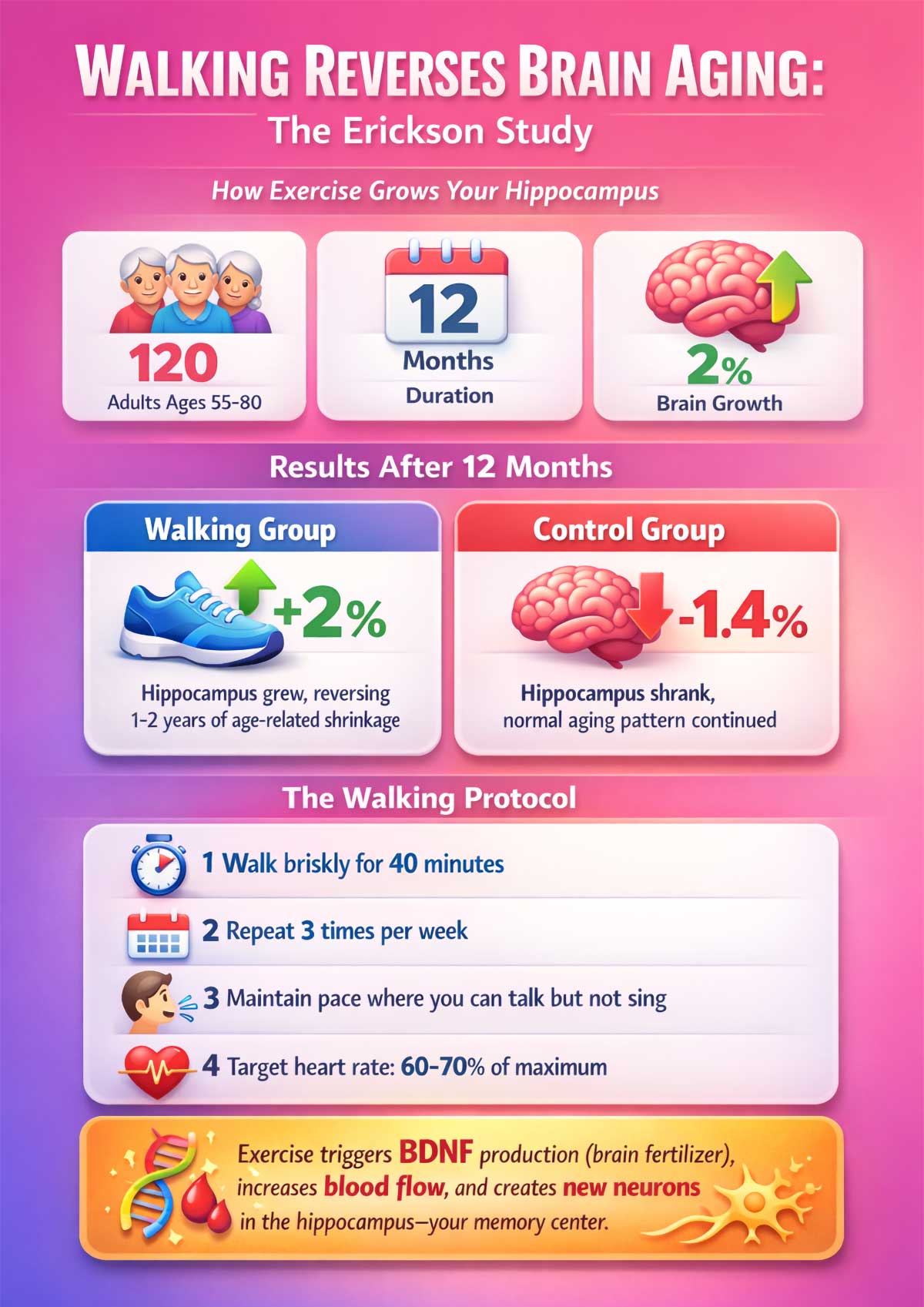
Why Walking Works:
The magic isn’t in the activity itself. It’s in what happens to your brain during aerobic exercise:
- Heart rate increases, pushing more blood to the brain
- Blood carries oxygen and nutrients brain cells need
- Exercise triggers BDNF release, which helps neurons grow and connect
- New blood vessels form in the hippocampus
- Inflammation markers drop throughout the body
You don’t need a gym. You need consistency. The Erickson study participants walked at a pace where they could talk but not sing. That’s moderate intensity. Three days per week, 40 minutes each time. In one year, their brains physically changed.
Precision Matters: The MAPT Study’s Subgroup Surprise
The MAPT study followed 1,680 adults over three years. Everyone had memory complaints but no dementia. Researchers tested omega-3 supplements and lifestyle coaching in different combos.
The overall results looked disappointing at first. No big wins across the board. But when scientists dug into subgroups, patterns emerged.
People with low omega-3 levels at the start showed real improvement. So did people with amyloid buildup in their brains—an early warning sign of Alzheimer’s. The intervention didn’t help everyone equally. It helped the right people at the right time.
This teaches us something critical: your genetic makeup and current brain health determine how well interventions work. One-size-fits-all doesn’t apply to brain health. You need the right approach for your situation.
Who Benefits Most from Omega-3s:
The MAPT study revealed specific profiles:
| Your Profile | Likely Benefit | Action Step |
|---|---|---|
| Eat fish less than once per week | High | Add 2-3 servings of fatty fish weekly or take fish oil (1,000-2,000 mg EPA+DHA) |
| Family history of Alzheimer’s | High | Talk to doctor about amyloid testing and targeted intervention |
| Already eat fish 2+ times per week | Low to Moderate | Focus on other interventions; omega-3s less critical |
| Vegetarian or vegan | Moderate | Consider algae-based omega-3 supplements |
Best Food Sources of Omega-3s:
- Salmon: 2,000 mg per 3 oz serving
- Mackerel: 3,000 mg per 3 oz serving
- Sardines: 1,200 mg per 3 oz serving
- Walnuts: 2,500 mg per 1/4 cup
- Flaxseeds: 2,400 mg per tablespoon (ground)
- Chia seeds: 2,400 mg per tablespoon
The body converts plant-based omega-3s (ALA) to the active forms (EPA and DHA) at low rates—about 5-10%. Fish and fish oil provide EPA and DHA directly.
Exercise Dose: How Much Movement Changes Your Brain
Patricia Smith analyzed 29 studies with 2,049 older adults. She wanted to know: does exercise really improve thinking? And how much do you need?
The answer: yes, but the effects are modest when you average everyone together. Attention and processing speed improved most. Memory showed smaller gains.
Laura Baker’s study added detail. She had 33 people with mild cognitive problems exercise hard for six months. High-intensity aerobic work—the kind that makes you breathe heavy—improved executive function and delayed memory recall.
The biological changes were gender-specific. Women’s insulin sensitivity improved more. Their levels of a harmful brain protein called Aβ42 went up, which sounds bad but might signal better clearance. Men’s Aβ42 levels dropped. Different paths, similar outcomes.
Here’s the practical takeaway: aim for 150 minutes per week of moderate activity. That’s 30 minutes, five days per week. Or go harder for less time—vigorous exercise three times per week works too. Consistency matters more than intensity for most people.
Understanding Exercise Intensity:
Not all movement affects the brain equally. Intensity matters:
| Intensity Level | Heart Rate | How It Feels | Brain Benefits | Examples |
|---|---|---|---|---|
| Light | 50-60% max | Can sing | Minimal cognitive impact; good for recovery | Casual walking, easy yoga, stretching |
| Moderate | 60-70% max | Can talk, can’t sing | Strong cognitive benefits; best for most people | Brisk walking, water aerobics, doubles tennis |
| Vigorous | 70-85% max | Can only say a few words | Maximum benefits but harder to sustain | Jogging, swimming laps, cycling uphill |
| High-Intensity | 85-95% max | Can’t talk | Excellent benefits; requires fitness base | Sprinting, HIIT, competitive sports |
Calculate Your Target Heart Rate:
- Find your max: 220 minus your age
- Moderate zone: Multiply max by 0.60 and 0.70
- Vigorous zone: Multiply max by 0.70 and 0.85
Example for a 65-year-old:
- Max heart rate: 220 – 65 = 155 beats per minute
- Moderate zone: 93-109 bpm
- Vigorous zone: 109-132 bpm
The Gender Difference in Brain Response:
Baker’s study revealed important distinctions:
Women’s Response to Exercise:
- Greater improvements in insulin sensitivity
- Better glucose uptake in brain regions
- Increased Aβ42 in blood (suggests better clearance from brain)
- Stronger executive function gains
- More benefit from consistent moderate exercise
Men’s Response to Exercise:
- Decreased Aβ42 in blood (different clearance mechanism)
- Better cardiovascular improvements
- Stronger gains in processing speed
- More benefit from higher-intensity intervals
These differences likely relate to hormones, body composition, and metabolic factors. Both genders benefit, but through slightly different biological pathways.
Progressive Exercise Plan:
Start where you are and build gradually:
Month 1: Foundation
- Week 1-2: 15 minutes, 3 days per week, light to moderate
- Week 3-4: 20 minutes, 4 days per week, moderate
Month 2: Building
- Week 5-6: 25 minutes, 4 days per week, moderate
- Week 7-8: 30 minutes, 4 days per week, moderate
Month 3: Target Reached
- Week 9-12: 30 minutes, 5 days per week, moderate
Month 4+: Variation
- Add one vigorous day per week
- Or extend two sessions to 45 minutes
- Or add strength training twice per week
Exercise Types and Brain Benefits:
Different activities offer unique advantages:
Aerobic (Walking, Running, Cycling):
- Strongest evidence for hippocampal growth
- Best for processing speed and executive function
- Improves cardiovascular health
- Recommended: 150 min/week minimum
Strength Training (Weights, Resistance Bands):
- Improves executive function
- Builds muscle mass (fights age-related loss)
- Enhances insulin sensitivity
- Recommended: 2 sessions/week, 20-30 min
Coordination Activities (Dancing, Tai Chi):
- Combines physical and cognitive challenge
- Improves balance and fall prevention
- Enhances spatial memory
- Social benefits boost mood
- Recommended: 1-2 sessions/week
Yoga and Stretching:
- Reduces stress hormones
- Improves sleep quality
- Enhances flexibility
- Less direct cognitive benefit but supports other activities
- Recommended: 2-3 sessions/week for recovery
Overcoming Exercise Barriers:
Common obstacles and solutions:
“I don’t have time.”
- Break into 10-minute chunks throughout the day
- Three 10-minute walks equal one 30-minute session
- Walk during phone calls or lunch breaks
“I have joint pain.”
- Try water aerobics (buoyancy reduces impact)
- Use a recumbent bike
- Focus on swimming
“I get too tired.”
- Start at just 5 minutes and add 1 minute per week
- Exercise in the morning when energy is highest
- Check with doctor about fatigue causes
“It’s boring.”
- Vary your routes and activities
- Listen to audiobooks or podcasts
- Exercise with friends or groups
- Set small weekly goals
“I can’t afford a gym.”
- Walking is free
- Use YouTube for home workouts
- Try community center programs (often low-cost)
- Use household items as weights (soup cans, water bottles)
The best exercise is the one you’ll actually do. Find what you enjoy and build from there.
Rapid Results: The Fotuhi Program’s 12-Week Sprint
Can you see changes in just three months? Majid Fotuhi tested this with 127 people who noticed their thinking wasn’t as sharp as before. Average age: 62 years old.
The program was intense. Nutrition plans. Exercise schedules. Cognitive games. Stress reduction. Sleep optimization. Everything at once for 12 weeks.
The results: 84% of people improved. Their average score on standard cognitive tests went up by three points. Some participants agreed to brain scans. Those scans showed hippocampal growth in just 90 days.

This proves early intervention works fast. If you’re starting to notice problems—forgetting appointments, losing your train of thought, struggling with familiar tasks—the window for improvement is wide open. You don’t need years. You need commitment.
The Fotuhi Program Components:
Here’s what the intensive 12-week program included:
Nutrition (Daily):
- Mediterranean-style meals with detailed meal plans
- Omega-3 supplementation (2,000 mg EPA+DHA)
- Limit processed foods and added sugars
- Stay hydrated (8 glasses of water daily)
Exercise (5 days per week):
- 30 minutes of aerobic activity
- Heart rate at 60-80% of maximum
- Mix of walking, swimming, cycling
Cognitive Training (30 minutes, 5 days per week):
- Computer-based brain games
- Focus on memory, attention, processing speed
- Increase difficulty as performance improves
Sleep Optimization (Daily):
- 7-8 hours per night
- Consistent bedtime and wake time
- Screen-free hour before bed
- Cool, dark bedroom
Stress Management (Daily):
- 10-20 minutes of meditation or deep breathing
- Journaling or gratitude practice
- Social connection activities
Creating Your Own 12-Week Sprint:
You can adapt this approach without a formal program:
Weeks 1-4: Build the Foundation
- Start walking 20 minutes, 3 days per week
- Add one fish meal per week
- Set a consistent bedtime
- Try a free brain training app for 10 minutes daily
Weeks 5-8: Increase Intensity
- Walk 30 minutes, 5 days per week
- Add second fish meal and more vegetables
- Extend brain training to 20 minutes
- Add 5 minutes of meditation
Weeks 9-12: Optimize and Sustain
- Maintain 150 minutes of exercise weekly
- Follow Mediterranean eating pattern consistently
- Continue cognitive training with new challenges
- Track your progress and celebrate wins
The key is combining multiple interventions. One change helps. Five changes together produce measurable results in 90 days.
Sustaining Gains: The ADCS Prevention Trial
Short-term wins are great. But do they last? The ADCS Prevention Trial followed 170 adults for two full years. Everyone had memory worries but no diagnosis.
Half got a home-based exercise program: 150 minutes per week of moderate activity. Walking, swimming, biking—their choice. The other half continued their normal routines.
At 18 months, the exercise group scored 1.3 points better on cognitive tests. That difference sounds small until you realize it’s the gap between declining and staying stable. The benefits held through the entire 24 months.
This matters because brain health isn’t a quick fix. It’s a lifestyle. The study showed that sustainable, long-term habits protect your brain year after year.
Real-Life Improvements: The Clare Study
What about people already diagnosed with early dementia? Linda Clare worked with 69 people whose MMSE scores ranged from 20 to 24—low enough for a dementia diagnosis.
Instead of generic brain games, Clare’s team personalized the approach. What goals mattered to each person? Remembering grandkids’ names? Following recipes? Managing medications?
For eight weeks, participants worked on their specific goals with therapists. Then researchers checked back six months later. The results held up. People reached their personal goals. They felt more capable. Their families noticed real improvements.
This study shows that even after decline begins, targeted training can restore function. You might not reverse the underlying disease, but you can regain abilities that matter to your daily life.
Real Stories from the Clare Study:
The study documented specific improvements:
Margaret, 76: Wanted to make Sunday roast for her family again. After training, she successfully prepared the meal using memory aids and strategies. Six months later, she still cooked weekly family dinners.
John, 72: Goal was managing his medications independently. Learned to use a pill organizer and phone reminders. Went from missing doses 3-4 times per week to perfect compliance.
Sarah, 68: Struggled to remember her grandchildren’s names and recent conversations. Training focused on association techniques. She regained confidence in social situations and reduced anxiety about family visits.
The Goal-Setting Process:
Clare’s approach involved specific steps:
- Identify What Matters: Patient and family discuss 3-5 meaningful goals
- Break Down Tasks: Each goal splits into smaller, manageable steps
- Learn Strategies: Memory aids, environmental cues, routine building
- Practice Daily: 20-30 minutes of focused practice
- Adjust and Adapt: Weekly check-ins to modify strategies
- Involve Family: Teach supporters how to reinforce learning
Effective Memory Strategies:
The study taught participants proven techniques:
External Aids:
- Pill organizers with alarms
- Labeled photos of family members
- Checklists for daily tasks
- Calendar alerts on phones
- Sticky notes in key locations
Internal Strategies:
- Verbal rehearsal (repeating names aloud)
- Visual imagery (linking names to pictures)
- Chunking (grouping information)
- Association (connecting new info to known facts)
- Routine building (same tasks, same time, same place)
Environmental Modifications:
- Clear labels on drawers and cabinets
- Photos showing task steps
- Remove clutter from key areas
- Consistent placement of important items
- Good lighting in all rooms
Measuring Functional Improvement:
Clare used Goal Attainment Scaling, which tracks personal progress:
| Rating | Description | Example |
|---|---|---|
| -2 | Much worse than baseline | Can’t start the task anymore |
| -1 | Somewhat worse | Task takes twice as long, many errors |
| 0 | No change | Baseline performance maintained |
| +1 | Somewhat better | Task completed with fewer errors |
| +2 | Much better | Task completed independently, confidently |
Most participants scored +1 or +2 on their primary goals. This matters more than abstract test scores. Real life improved.
Quality of Life Changes:
The study measured several outcomes:
Patient Reports:
- 73% felt more confident in daily activities
- 68% reported less anxiety about memory
- 81% were satisfied with their progress
- 65% maintained gains at 6 months
Family Reports:
- 70% saw meaningful improvements in daily function
- 62% reported less caregiver stress
- 75% felt the training was worthwhile
- 58% noticed better mood in their loved one
Applying This Approach at Home:
You can use goal-focused training without a formal program:
Week 1: Identify One Specific Goal
- Pick something concrete: making coffee, remembering appointments, following a recipe
- Make it measurable: can do it independently, with one cue, or with help
Week 2-3: Break It Down
- List every step of the task
- Identify where you struggle
- Create aids for trouble spots
Week 4-6: Practice Daily
- Do the task same time each day
- Use your memory aids consistently
- Track success and challenges
Week 7-8: Reduce Supports
- Slowly remove aids you don’t need
- Build confidence in your ability
- Celebrate progress
Month 3+: Maintain and Expand
- Keep practicing your mastered goal
- Add a new goal using the same process
The key is focusing on function that matters to you, not abstract memory tests.
Your Action Plan: Five Data-Backed Steps
Based on 3,500+ adults across eight trials, here’s what the science supports:
1. Move Your Body Daily
Aim for 150 minutes per week of activity that raises your heart rate. Walking counts. So does dancing, swimming, or biking. The hippocampus grows in response to aerobic exercise.
Weekly Exercise Template:
- Monday: 30-minute brisk walk
- Tuesday: Rest or light stretching
- Wednesday: 30-minute swim or bike ride
- Thursday: Rest or yoga
- Friday: 30-minute dance class or hiking
- Saturday: 30-minute gardening or active hobby
- Sunday: 30-minute family walk
Start where you are. Add five minutes per week until you hit your goal. Track your heart rate—aim for 50-70% of your max during moderate exercise. Calculate your max: subtract your age from 220.
2. Eat to Feed Your Brain
The FINGER trial used a diet rich in vegetables, fish, whole grains, and healthy fats. Think Mediterranean style. Omega-3s matter, especially if your diet’s been low in fish.
Brain-Healthy Meal Pattern:
Breakfast: Steel-cut oats with blueberries, walnuts, and cinnamon. Greek yogurt on the side.
Lunch: Large salad with leafy greens, chickpeas, cherry tomatoes, cucumber, olive oil, and lemon. Whole grain bread.
Dinner: Baked salmon with roasted Brussels sprouts and quinoa. Side of mixed berries.
Snacks: Handful of almonds, apple slices with almond butter, or carrot sticks with hummus.
Key Foods to Include Daily:
- Leafy greens: spinach, kale, arugula
- Berries: blueberries, strawberries, blackberries
- Fatty fish: salmon, mackerel, sardines (2-3 times per week)
- Nuts and seeds: walnuts, almonds, flaxseeds
- Olive oil: 2-3 tablespoons for cooking and dressing
- Whole grains: oats, quinoa, brown rice, whole wheat
3. Challenge Your Mind
Brain training isn’t just crossword puzzles. Learn a language. Take up an instrument. Try new recipes. The key is novelty and difficulty. If it’s easy, your brain isn’t growing.
Monthly Brain Challenge Ideas:
- Week 1: Learn 20 words in a new language
- Week 2: Try three new recipes from a different cuisine
- Week 3: Practice a new skill (instrument, drawing, knitting)
- Week 4: Teach someone else what you learned
Combine physical and mental activity when possible. Learning dance steps works your body and brain together.
4. Optimize Sleep and Stress
The Fotuhi program made this a priority. Poor sleep disrupts memory formation. Chronic stress shrinks the hippocampus. Address both.
Sleep Hygiene Checklist:
- Set a consistent bedtime (within 30 minutes each night)
- Keep your bedroom cool (65-68°F works for most people)
- Block out light with curtains or an eye mask
- Stop screens 60 minutes before bed
- Avoid caffeine after 2 PM
- Try a warm bath or shower 90 minutes before sleep
Daily Stress Management:
- Morning: 5 minutes of deep breathing
- Midday: 10-minute walk outside
- Evening: 10 minutes of meditation or journaling
That might mean fixing sleep apnea, learning meditation, or getting therapy for anxiety. Talk to your doctor if you snore loudly or wake up tired despite sleeping 7-8 hours.
5. Monitor Your Health Markers
High blood pressure, diabetes, and high cholesterol all speed brain decline. Work with your doctor to keep these in check.
Target Numbers for Brain Health:
| Health Marker | Optimal Range | Why It Matters |
|---|---|---|
| Blood Pressure | Below 120/80 mmHg | High BP damages small brain vessels |
| Fasting Blood Sugar | 70-99 mg/dL | High sugar harms memory centers |
| HbA1c | Below 5.7% | Shows 3-month blood sugar control |
| LDL Cholesterol | Below 100 mg/dL | High LDL increases dementia risk |
| HDL Cholesterol | Above 60 mg/dL | HDL protects brain vessels |
| BMI | 18.5-24.9 | Obesity doubles dementia risk |
| Waist Size | Men <40 inches, Women <35 inches | Belly fat produces harmful proteins |
Get these checked yearly. Small improvements in vascular health produce measurable cognitive benefits. If any number sits outside the optimal range, ask your doctor about treatment options.
The Window Is Wider Than We Thought
Here’s the truth: cognitive decline isn’t always a one-way trip. The brain retains remarkable repair capacity well into older age.
Early intervention matters most. If you’re noticing changes—even small ones—act now. The people who improved most in these studies caught problems early and addressed multiple factors at once.
You won’t find a pill that fixes everything. But you do have tools that work. Movement, nutrition, mental challenge, sleep, and stress control all change the brain in measurable ways.
The 3,500 adults in these trials showed us what’s possible. Some grew their hippocampus. Some improved their test scores. Some regained abilities they thought were gone forever.
Your brain is still plastic. Still capable of change. Still worth fighting for.
The question isn’t whether cognitive decline can be reversed. These eight studies answered that: yes, for many people, under the right conditions.
The real question is: will you give your brain what it needs to heal?
Common Myths About Brain Decline
Myth 1: “Brain decline is genetic. I can’t change my fate.”
Reality: Genetics account for only 20-30% of dementia risk. The FINGER trial included people with high genetic risk. They still improved with lifestyle changes. Even if Alzheimer’s runs in your family, your daily habits strongly influence whether and when symptoms appear.
Myth 2: “Memory loss is a normal part of aging.”
Reality: Some slowing is normal. Forgetting where you put your keys occasionally happens to everyone. But significant memory problems—forgetting important events, getting lost in familiar places, repeating questions—are not normal aging. They signal a problem you can address.
Myth 3: “It’s too late to help once you have symptoms.”
Reality: The Clare study proved otherwise. People with diagnosed dementia improved their daily function. The Fotuhi program showed rapid gains in people already experiencing decline. Early is better, but late isn’t too late.
Myth 4: “Brain games prevent Alzheimer’s.”
Reality: Computer brain games alone show weak benefits. They make you better at the games, not necessarily at real-life tasks. The FINGER trial worked because brain training combined with exercise, diet, and health monitoring. Multidomain beats single interventions every time.
Myth 5: “I’m too old to start exercising.”
Reality: The Erickson study participants averaged 67 years old and were sedentary. They still grew their hippocampus. The oldest participant who improved was 80. Your brain responds to exercise at any age. Start gently and build gradually.
Myth 6: “Supplements can reverse brain decline.”
Reality: The MAPT study showed omega-3s help specific subgroups, not everyone. No supplement works as well as comprehensive lifestyle change. Most “brain health” supplements lack strong evidence. Focus on food first, supplements second, and only under doctor guidance.
Myth 7: “If I don’t have symptoms, I don’t need to worry.”
Reality: Brain changes begin 10-20 years before symptoms appear. The FINGER trial enrolled people with risk factors but no symptoms. Prevention works better than treatment. Start building brain health habits now, regardless of your current function.
Risk Factors You Can Control
Understanding your risk helps you prioritize interventions:
| Risk Factor | Impact on Dementia Risk | Action Steps |
|---|---|---|
| Physical Inactivity | Increases risk 82% | Start with 10 min walks, build to 150 min/week |
| High Blood Pressure | Increases risk 60% | Monitor at home, take prescribed meds, reduce sodium |
| Obesity (BMI >30) | Doubles risk | Lose 5-10% body weight through diet and exercise |
| Type 2 Diabetes | Increases risk 73% | Control blood sugar, take medication, eat low-glycemic foods |
| Smoking | Increases risk 79% | Quit now—brain benefits appear within months |
| Depression | Increases risk 65% | Seek therapy, consider medication, practice stress management |
| Social Isolation | Increases risk 57% | Join groups, volunteer, schedule regular social time |
| Hearing Loss | Increases risk 94% | Get hearing tested, use hearing aids if needed |
| Low Education | Increases risk 59% | Continue learning throughout life—take classes, read, learn skills |
| Excessive Alcohol | Increases risk 22% | Limit to 1 drink/day for women, 2 for men |
| Poor Sleep | Increases risk 30% | Treat sleep apnea, maintain sleep schedule, aim for 7-8 hours |
| Head Injuries | Increases risk 63% | Wear helmets, prevent falls, avoid contact sports |
Calculate Your Personal Risk:
Count how many risk factors apply to you:
- 0-2 factors: Low risk—focus on prevention
- 3-4 factors: Moderate risk—start interventions now
- 5+ factors: High risk—seek medical guidance and aggressive lifestyle change
Each factor you improve lowers your risk. You don’t need to fix everything at once. Pick one factor this month and address it.
The Science of Brain Plasticity
Why can brains change at all? Understanding the biology helps you believe change is possible.
Neuroplasticity Basics:
Your brain contains about 86 billion neurons. Each neuron connects to thousands of others through synapses. These connections change constantly based on your experiences.
When you learn something new:
- Neurons fire together repeatedly
- Connections between them strengthen
- New synapses form
- Supporting brain cells multiply
- Blood vessels grow to feed the area
This process—neuroplasticity—continues throughout life. It slows with age but never stops completely.
Neurogenesis: Growing New Brain Cells
For decades, scientists believed adults couldn’t grow new neurons. That changed in the 1990s. We now know the hippocampus produces new neurons daily, even in older adults.
Exercise triggers neurogenesis through several pathways:
- Increased BDNF production (growth factor for neurons)
- Better blood flow delivering oxygen and nutrients
- Reduced inflammation that damages brain cells
- Improved insulin sensitivity supporting cell metabolism
- Increased production of new blood vessels
The Erickson study showed this process clearly. Walkers grew their hippocampus because they literally created new neurons and supporting structures.
Synaptic Pruning: Use It or Lose It
Your brain is efficient. Connections you don’t use get pruned away. Connections you use regularly get stronger.
This explains why cognitive training works. The FINGER trial participants did computer tasks three times per week. They strengthened specific neural pathways through repeated practice. The brain responds: “This matters, keep these connections strong.”
Factors That Enhance Plasticity:
Certain conditions make your brain more plastic:
Novelty: New experiences create stronger changes than familiar ones. Learning Italian creates more synapses than doing crosswords you’ve mastered.
Challenge: Tasks at the edge of your ability drive growth. Too easy and there’s no stimulus. Too hard and you give up.
Multisensory: Activities engaging multiple senses (vision, hearing, touch, movement) create richer neural networks.
Emotional Engagement: Things you care about create stronger memories and connections.
Social Interaction: Social activities engage multiple brain regions simultaneously.
Physical Movement: Exercise primes the brain for learning and memory formation.
Age-Related Changes:
Plasticity does decline with age, but less than you might think:
- Young adults: Maximum plasticity, fast learning
- Middle age (40-60): Slightly slower but still strong
- Older adults (60-80): Reduced but significant capacity
- Very old (80+): Slower changes but still possible
The key difference: older brains need more repetition and time to form new connections. They still form them. Be patient with yourself.
Supplements: What Works, What Doesn’t
The market floods us with “brain health” pills. Most lack evidence. Here’s what the research actually shows:
Strong Evidence:
Omega-3 Fatty Acids (EPA+DHA):
- Effective dose: 1,000-2,000 mg combined EPA+DHA daily
- Best for: People with low dietary intake, family history of dementia
- Evidence: MAPT study showed benefits in targeted groups
- Choose: Molecularly distilled fish oil or algae-based for vegetarians
- Cost: $15-30 per month
Moderate Evidence:
Vitamin D:
- Many older adults are deficient
- Low levels correlate with cognitive decline
- Aim for blood level: 30-50 ng/mL
- Dose: 1,000-2,000 IU daily, adjust based on blood test
- Cost: $5-10 per month
B Vitamins (B6, B12, Folate):
- Important for people with high homocysteine levels
- May slow brain atrophy in people with MCI
- Best from food, but supplements help if deficient
- Check levels before supplementing
- Cost: $10-15 per month
Weak or No Evidence:
Ginkgo Biloba: Large studies show no benefit for preventing dementia
Phosphatidylserine: Minimal effects in rigorous trials
Prevagen: No credible evidence despite marketing claims
Coconut Oil/MCT Oil: Lacks support from controlled trials
Huperzine A: Insufficient evidence, potential side effects
The Bottom Line on Supplements:
Focus on food first. The FINGER diet provides most nutrients you need. Consider supplements only if:
- You have documented deficiencies
- You can’t get enough from food (omega-3s for vegetarians)
- Your doctor recommends them based on your specific risk factors
Save your money for high-quality food and a gym membership. They work better.
Quick Reference: Eight Studies at a Glance
Brain-Healthy Recipe: Mediterranean Salmon Bowl
This meal combines multiple brain-boosting foods from the FINGER trial diet. It takes 25 minutes and feeds four people.
Ingredients:
For the salmon:
- 4 salmon fillets (4-6 oz each)
- 2 tablespoons olive oil
- 1 teaspoon dried oregano
- Juice of half a lemon
- Salt and pepper to taste
For the bowl:
- 2 cups cooked quinoa
- 4 cups mixed greens (spinach, arugula, kale)
- 1 cup cherry tomatoes, halved
- 1 cucumber, diced
- 1 cup chickpeas, drained and rinsed
- 1/4 cup walnuts, chopped
- 1/4 cup crumbled feta cheese
For the dressing:
- 3 tablespoons olive oil
- 1 tablespoon lemon juice
- 1 teaspoon honey
- 1 clove garlic, minced
- Salt and pepper to taste
Instructions:
- Heat oven to 400°F. Line a baking sheet with parchment paper.
- Place salmon on the sheet. Drizzle with olive oil and lemon juice. Sprinkle with oregano, salt, and pepper.
- Bake for 12-15 minutes until salmon flakes easily with a fork.
- While salmon cooks, mix dressing ingredients in a small bowl. Whisk until combined.
- Divide quinoa among four bowls. Top with greens, tomatoes, cucumber, and chickpeas.
- Place one salmon fillet in each bowl.
- Drizzle with dressing. Sprinkle walnuts and feta on top.
Brain Benefits Per Serving:
- Omega-3 fatty acids from salmon and walnuts
- Antioxidants from vegetables and olive oil
- Protein for stable blood sugar
- Fiber from quinoa and vegetables
- B vitamins from greens and fish
Nutritional Breakdown (per serving):
- Calories: 520
- Protein: 38g
- Fat: 26g (heart-healthy fats)
- Carbs: 35g
- Fiber: 8g
- Omega-3s: 2,200mg
- Vitamin E: 4mg
- B vitamins: High in B6, B12, folate
Recipe Variations:
Budget-Friendly Version:
- Replace salmon with canned sardines or mackerel ($2 vs $8)
- Use frozen spinach instead of mixed greens
- Swap feta for cottage cheese
- Cost per serving drops from $6 to $2.50
Vegetarian Version:
- Replace salmon with extra chickpeas and 1/4 cup hemp seeds
- Add 1 cup edamame for protein
- Include 2 tablespoons ground flaxseed
- Omega-3s: 2,000mg from plant sources
Quick Version (15 minutes):
- Use pre-cooked quinoa pouches
- Buy pre-washed greens
- Use rotisserie salmon from grocery
- Use bottled lemon vinaigrette
Meal Prep Tips:
Make components ahead:
- Cook quinoa: stores 5 days in fridge
- Chop vegetables: stores 3 days in containers
- Make dressing: lasts 1 week in jar
- Bake salmon fresh or use canned wild salmon
Additional Brain-Healthy Recipes:
Berry-Walnut Breakfast Bowl
Ingredients (serves 2):
- 1 cup steel-cut oats
- 2 cups water or milk
- 1 cup mixed berries (blueberries, strawberries)
- 1/4 cup walnuts, chopped
- 2 tablespoons ground flaxseed
- 1 teaspoon cinnamon
- 1 tablespoon honey
Instructions:
- Cook oats in water according to package directions (20 minutes).
- Top with berries, walnuts, and flaxseed.
- Sprinkle cinnamon and drizzle honey.
Brain benefits: Anthocyanins from berries, omega-3s from walnuts and flax, sustained energy from oats.
Spinach and White Bean Soup
Ingredients (serves 4):
- 2 tablespoons olive oil
- 1 onion, diced
- 3 garlic cloves, minced
- 4 cups low-sodium vegetable broth
- 2 cans white beans, drained
- 4 cups fresh spinach
- 1 can diced tomatoes
- 1 teaspoon dried basil
- Juice of 1 lemon
Instructions:
- Heat olive oil in pot. Cook onion until soft (5 minutes).
- Add garlic, cook 1 minute.
- Add broth, beans, tomatoes, and basil. Simmer 15 minutes.
- Stir in spinach until wilted.
- Add lemon juice. Season with salt and pepper.
Brain benefits: Folate from spinach and beans, antioxidants from tomatoes, anti-inflammatory compounds from olive oil.
Turmeric-Ginger Smoothie
Ingredients (serves 2):
- 1 banana, frozen
- 1 cup mango chunks, frozen
- 1 cup unsweetened almond milk
- 1 teaspoon fresh ginger, grated
- 1/2 teaspoon turmeric powder
- 1 tablespoon almond butter
- Pinch of black pepper
- 1/2 cup Greek yogurt
Instructions:
- Blend all ingredients until smooth.
- Add ice if needed for thickness.
Brain benefits: Curcumin from turmeric (black pepper increases absorption 2000%), anti-inflammatory compounds from ginger, potassium from banana.
Weekly Meal Planning Template:
| Day | Breakfast | Lunch | Dinner | Brain Focus |
|---|---|---|---|---|
| Monday | Berry-Walnut Bowl | Spinach-Bean Soup | Mediterranean Salmon Bowl | Omega-3 loading day |
| Tuesday | Greek yogurt with walnuts | Leftover salmon bowl | Grilled chicken with roasted vegetables | Variety day |
| Wednesday | Turmeric smoothie | Large salad with chickpeas | Baked cod with quinoa | Anti-inflammatory focus |
| Thursday | Oatmeal with berries | Leftover soup | Turkey meatballs with whole wheat pasta | B-vitamin day |
| Friday | Egg scramble with spinach | Tuna salad on greens | Mediterranean salmon bowl | Omega-3 day |
| Saturday | Weekend treat (whole grain pancakes) | Veggie stir-fry | Restaurant meal (choose fish if possible) | Flexibility |
| Sunday | Avocado toast on whole grain | Homemade vegetable soup | Meal prep for week ahead | Preparation day |
This pattern ensures:
- Omega-3s: 2-3 times per week
- Vegetables: Every meal
- Whole grains: Daily
- Variety: Different foods each day
- Sustainability: Realistic for long-term adherence
Understanding Your Cognitive Baseline
Before you start any intervention, know where you stand. This helps you track progress and celebrate wins.
Simple Self-Assessment Questions:
Ask yourself these monthly:
- Do I forget appointments without checking my calendar?
- Do I lose my train of thought during conversations?
- Do I struggle to follow recipes I’ve made before?
- Do I have trouble finding words I know?
- Do I get lost in familiar places?
- Do I repeat questions or stories without realizing it?
If you answer yes to two or more, talk to your doctor. Early detection matters. The people in these studies who improved most caught changes early.
Tracking Tools:
Keep a simple journal:
- Week 1: Note your baseline (memory lapses per day, mood, energy)
- Monthly: Reassess the questions above
- Quarterly: Try an online cognitive test (many are free)
- Yearly: Schedule a checkup with your doctor
Small improvements count. If you went from forgetting three appointments per month to just one, that’s progress worth celebrating.
When to Seek Professional Help
These studies show self-directed interventions work. But some situations need medical attention:
Red Flags:
- Memory problems that interfere with daily life
- Getting lost in familiar places
- Trouble with basic tasks you’ve done for years
- Personality changes your family notices
- Forgetting recent events completely
- Difficulty with money management or bills
Don’t wait if you see these signs. The window for reversal is widest early. Every month matters when it comes to intervention timing.
What to Ask Your Doctor:
- “Can we test my cognitive function?”
- “What’s my dementia risk based on my health markers?”
- “Should I see a neurologist or specialist?”
- “Are any of my medications affecting my memory?”
- “What local programs support brain health?”
Bring a family member to appointments. They often notice changes you might miss or minimize.


