Memory lapses happen to everyone. But when do these moments cross the line from typical forgetfulness to a real problem? The answer isn’t always simple.
Your brain stores and retrieves information through a complex network of connections. When something disrupts this process, memory suffers. The good news? Many of these disruptions can be fixed.
This guide breaks down 12 factors that affect memory. Some you can control today. Others need medical help. Either way, knowing what’s happening inside your brain is the first step to getting it back on track.
The Difference Between Normal Forgetting and Memory Loss
Your brain isn’t a filing cabinet. It’s more like a busy office where information gets sorted, stored, and pulled out when you need it.
Normal forgetting happens when the retrieval system has a hiccup. You know the information is there. You just can’t access it right now. This happens to everyone.
Memory loss is different. The data itself becomes damaged or never gets stored properly in the first place. This affects your daily life and gets worse over time.
Think of it this way: forgetting where you parked is normal. Forgetting you drove to the store isn’t.
The Lifestyle Disruptors: Factors You Can Change Right Now
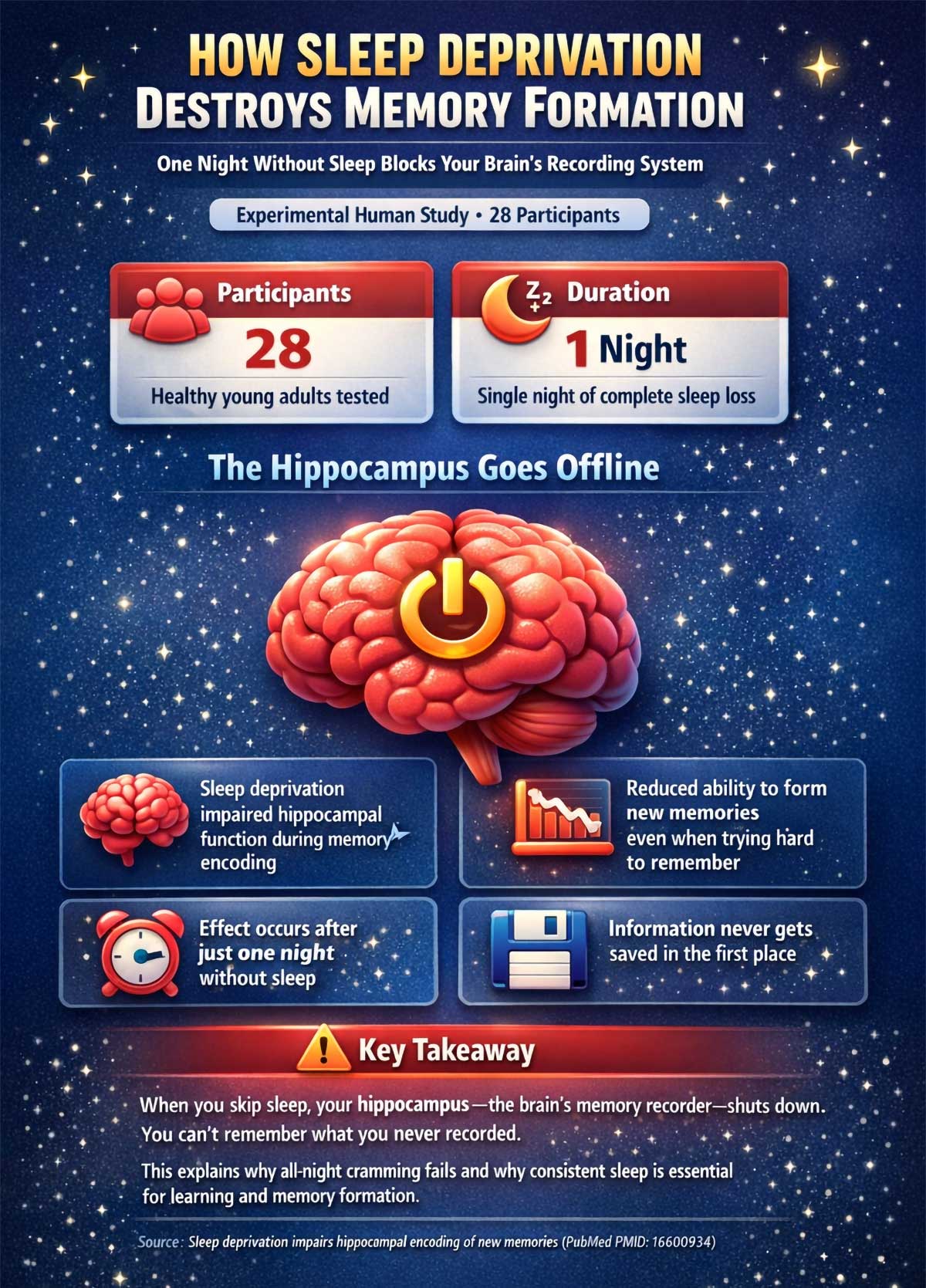
1. Acute Sleep Deprivation: When Your Brain Goes Offline
One night of bad sleep does more than make you groggy. It actually blocks your brain from forming new memories.
Your hippocampus acts like a recorder, capturing experiences and converting them into long-term storage. But when you skip sleep, this recorder shuts down.
A study of 28 healthy young adults found that a single night without sleep impaired their ability to encode new memories. The hippocampus simply couldn’t do its job during the encoding phase.
The result? Even if you try hard to remember something, your brain never saved it in the first place.
This explains why cramming all night before an exam backfires. Your brain needs sleep to lock in what you learned.
And chronic sleep deprivation? The damage compounds night after night, affecting both memory formation and the brain’s ability to clear out toxic proteins that build up during waking hours.
What you can do: Aim for 7-9 hours of quality sleep. If you’re preparing for something important, sleep on it. Literally.
2. Chronic Stress: The Brain Shrinker
Stress doesn’t just feel bad. It physically changes your brain.
When you’re stressed, your body pumps out cortisol. This hormone helps you deal with threats in the short term. But when cortisol stays high for weeks or months, it starts eating away at brain tissue.
Researchers measured cortisol levels and brain volume in adults aged 18-50. Those with higher cortisol had lower total brain volume. Their memory performance suffered too, especially among women.
The damage hits the hippocampus first. This region shrinks under constant stress, making it harder to form and recall memories.
Chronic stress also interferes with focus. When your mind is racing with worries, you can’t pay attention to what’s happening around you. If you don’t encode the memory in the first place, you can’t recall it later.
What you can do: Find stress outlets that work for you. Exercise, meditation, or talking to a friend can all help lower cortisol levels.
3. Alcohol: The Risky Middle Ground
The relationship between alcohol and memory isn’t straightforward.
You might think any drinking is bad for your brain. Or that a glass of wine protects it. Both views are too simple.
A 23-year study of over 9,000 adults aged 35-55 revealed a J-shaped risk curve. Both people who never drank alcohol and heavy drinkers (more than 14 units per week) faced higher rates of memory problems compared to moderate drinkers.
Why? Heavy drinking damages brain cells directly and shrinks the hippocampus. But complete abstinence might miss out on some protective effects seen with light to moderate use.
One unit equals about half a pint of beer or a small glass of wine. Drinking more than 14 units weekly puts you in the danger zone.
What you can do: If you drink, keep it moderate. If you don’t drink, don’t start just for brain health. The risks often outweigh the benefits.
The Silent Clinical Influencers: Hidden Medical Factors
4. Untreated High Blood Pressure: The Midlife Connection
Your blood pressure in your 40s predicts your memory in your 70s.
This might sound far-fetched, but the science is clear. High blood pressure damages tiny blood vessels in your brain. Over years and decades, this damage accumulates.
The Honolulu-Asia Aging Study tracked Japanese-American men for over 25 years. Those with untreated high blood pressure in midlife showed significantly more brain lesions and thinking problems in late life.
This is what makes high blood pressure so dangerous. You can feel perfectly fine in your 40s while setting the stage for memory problems decades later. The damage is silent but builds up over time.
These lesions are like scars on your brain. They interrupt the flow of signals between cells. Memory circuits break down.
The scary part? High blood pressure has no symptoms. You can feel fine while damage builds up inside.
What you can do: Get your blood pressure checked regularly, especially if you’re over 40. If it’s high, work with your doctor to bring it down. The sooner you act, the more brain damage you can prevent.
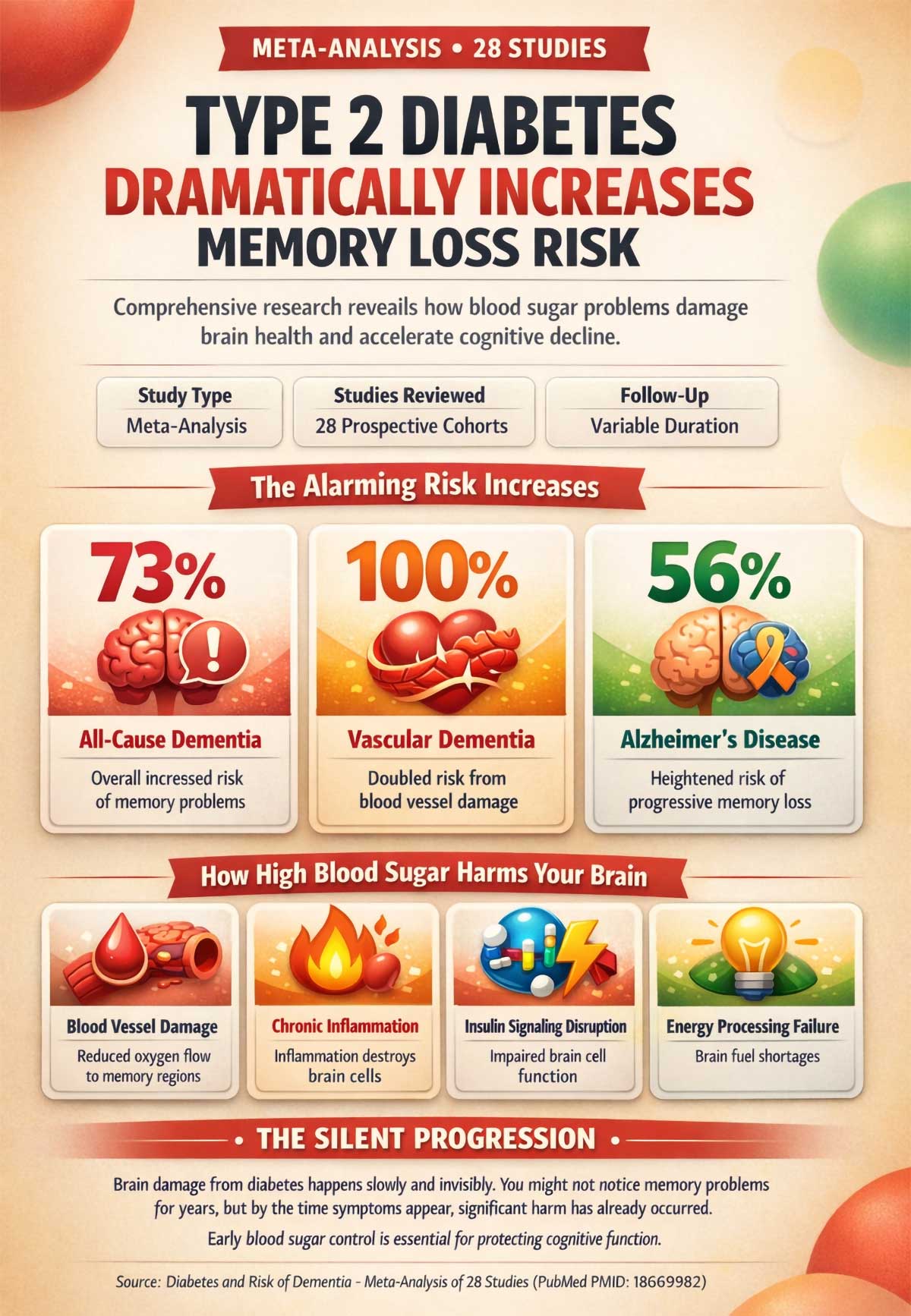
5. Type 2 Diabetes: When Blood Sugar Hurts Your Brain
Diabetes doesn’t just affect your blood sugar. It affects your brain too.
A major review of 28 studies found that people with diabetes face a 73% increased risk of memory problems overall. The risk jumps to 100% for vascular-related issues and 56% for Alzheimer’s specifically.
How does high blood sugar damage memory? Several ways:
- It harms blood vessels in the brain, reducing oxygen flow
- It causes inflammation that kills brain cells
- It interferes with insulin signaling, which brain cells need to function
Your brain uses massive amounts of energy. When diabetes disrupts how cells process fuel, memory suffers.
The damage happens slowly. You might not notice problems for years. But by the time symptoms appear, significant harm has already occurred.
What you can do: Control your blood sugar through diet, exercise, and medication if needed. Monitor your A1C levels. Keeping diabetes in check protects your brain as much as your heart.
6. Sleep Apnea: The Oxygen Thief
Sleep apnea does more than make you snore. It slowly suffocates your brain.
When you stop breathing during sleep, oxygen levels drop. Your brain cells can’t survive without oxygen. Do this dozens to hundreds of times a night, depending on severity, and brain tissue starts to die.
A study using MRI scans found that middle-aged and older adults with sleep apnea had measurable brain tissue loss. The damage showed up in regions that control memory and thinking. Worse sleep apnea meant worse tissue loss.
Many people don’t know they have sleep apnea. They just know they’re tired all the time. Their partner might complain about loud snoring. But the real damage happens invisibly, night after night.
What you can do: If you snore loudly, feel exhausted despite sleeping, or wake up gasping, get tested for sleep apnea. Treatment with a CPAP machine can stop the damage and improve memory.
Psychological and Social Pillars: The Mind-Body Connection
7. Depression: More Than Just Sadness
Depression affects how you feel. It also affects how you think.
People with a history of depression face double the risk of developing serious memory problems later in life. A review of 23 studies confirmed this link across thousands of adults.
Late-life depression is an especially strong warning sign. It might actually be an early symptom of brain changes already happening.
Depression can also create what doctors call “pseudodementia.” Your memory seems terrible, but it’s actually the depression interfering with focus and recall. Treat the depression, and memory often improves.
The connection works both ways. Depression changes brain chemistry and structure. It reduces the size of the hippocampus. It disrupts neurotransmitters that help form and retrieve memories.
But here’s the key difference: depression-related memory problems usually improve with treatment. True brain disease doesn’t.
What you can do: Don’t dismiss depression as “just” a mood issue. Get help. Therapy and medication can protect your brain as well as your mental health.
8. Social Isolation: The Loneliness Tax
Humans are social creatures. Our brains need interaction to stay sharp.
A review of 19 studies found that social isolation and loneliness increase the risk of memory decline by about 50%. That’s huge.
Why does loneliness hurt the brain? Your social connections literally build and maintain brain pathways. When you talk, laugh, argue, and connect with others, you activate complex thinking processes.
These interactions keep synapses firing. They maintain what scientists call “synaptic density” – the richness of connections between brain cells.
Isolated people lose this stimulation. Their brains start to prune away unused pathways. Memory circuits weaken.
Social connection also protects against depression and gives you reasons to stay active and engaged with life. These factors compound the brain benefits.
What you can do: Make social time a priority. Join a club. Volunteer. Call friends regularly. Even small interactions add up to protect your brain.

Nutritional and Chemical Factors: What You Put In Matters
9. Vitamin B12 Deficiency: The Nerve Protector
Your brain needs B12 to function. Without enough, it starts to deteriorate.
A 5-year study of 107 older adults measured B12 levels and tracked brain changes. Those with lower B12 experienced faster brain shrinkage and memory decline.
B12 protects the myelin sheaths that wrap around nerve fibers. Think of myelin like insulation on electrical wires. Without it, signals get weak and garbled.
B12 deficiency is surprisingly common, especially in older adults and people who don’t eat animal products. Your stomach produces less acid as you age, which you need to absorb B12 from food.
The tricky part? Symptoms develop slowly. You might feel tired or foggy for years before realizing something’s wrong.
What you can do: Get your B12 levels checked, especially if you’re over 50 or vegetarian. If you’re low, supplements or injections can restore levels quickly. This is one cause of memory loss that’s truly reversible.
10. Thyroid Problems: The Metabolic Slowdown
Your thyroid controls your body’s metabolism. That includes your brain’s metabolism.
When your thyroid doesn’t make enough hormone, everything slows down. Your thinking gets sluggish. Your memory suffers.
A 12.7-year study of 1,864 adults over 65 found that subclinical hypothyroidism increased risk for memory problems. This is when your thyroid is struggling but not failing completely. Your TSH levels creep up (≥10 mIU/L), signaling your body is pushing hard to get thyroid hormone production going.
Many doctors miss this because symptoms are subtle. You might just feel a bit off. Cold. Tired. Forgetful.
But inside, your brain cells are struggling to get the energy they need to fire properly.
What you can do: Ask your doctor to check your thyroid function, including TSH levels. If your thyroid is underactive, medication can restore normal function and improve memory.
11. Common Medications: The Hidden Risk
Some medications you take every day might be hurting your memory.
A 7-year study of 3,434 adults over 65 found that high cumulative exposure to anticholinergic drugs increased the risk of serious memory problems. The strongest links appeared with antidepressants, antihistamines, and bladder control medications.
Anticholinergic means these drugs block acetylcholine, a brain chemical vital for memory. Block it long enough, and memory suffers.
Many people take these medications without realizing the cognitive cost:
- Over-the-counter sleep aids (often contain diphenhydramine)
- Allergy medications (like Benadryl)
- Certain antidepressants (especially older tricyclics)
- Overactive bladder medications
- Some muscle relaxants
One pill won’t cause problems. But take them daily for years? The effects add up.
This is especially important for older adults taking multiple medications. The anticholinergic effects can add up across different drugs, creating a cognitive burden that no single medication would cause alone.
What you can do: Review all your medications with your doctor, including over-the-counter ones. Ask if any have anticholinergic effects. Your doctor might be able to switch you to safer alternatives.
The Physical Connection: Move Your Body, Boost Your Brain
12. Physical Inactivity: The Sedentary Brain
Sitting still doesn’t just weaken your muscles. It weakens your mind.
A comprehensive review of multiple studies found that physical inactivity raises the risk of memory decline by 82%. On the flip side, exercise interventions showed clear cognitive benefits.
When you move, you don’t just burn calories. You grow your brain.
Exercise increases blood flow to the hippocampus. It triggers the release of growth factors that help brain cells multiply and form new connections. This process is called neuroplasticity – your brain’s ability to reshape itself.
Even moderate activity helps. You don’t need to run marathons. Walking briskly for 30 minutes most days of the week provides significant protection.
Physical activity also reduces many other risk factors for memory loss. It lowers blood pressure. It helps control blood sugar. It reduces stress and improves sleep.
What you can do: Start moving more today. Take the stairs. Walk during lunch breaks. Find an activity you enjoy and stick with it. Your brain will thank you.

When Should You Worry?
Not every memory slip needs a doctor visit. So how do you know when to seek help?
Ask yourself these questions:
Frequency: Does this happen occasionally or daily?
An occasional forgotten name is normal. Forgetting conversations that happened an hour ago isn’t.
Severity: Does it affect your daily life?
Forgetting where you put your keys is annoying. Forgetting how to use your keys is concerning.
Progression: Is it getting worse?
Everyone has memory lapses. But if you notice a steady decline over months, that’s a red flag.
Impact: Are other people noticing?
If friends or family express concern about your memory, listen. They see patterns you might miss.
Pattern: Does forgetting follow a pattern?
Always recent events but not old ones? Always names but not faces? Always appointments but not skills? Consistent patterns in what you forget can help doctors identify specific causes.
Age: How old are you?
Memory problems at 30 warrant more concern than at 70. But even in older age, significant decline isn’t normal.
Take Action: Steps You Can Start Today
Memory loss has many causes. That means you have many ways to fight back.
Here’s what you can do right now:
Sleep better. Turn off screens an hour before bed. Keep your room cool and dark. Make sleep a priority.
Manage stress. Find what calms you. Exercise, meditation, time in nature, or talking to loved ones all help.
Stay social. Schedule regular time with friends. Join groups. Volunteer. Keep your social brain active.
Move your body. Aim for 150 minutes of moderate activity per week. Walk, dance, garden – anything that gets you moving.
Check your health. Get your blood pressure, blood sugar, thyroid, and B12 levels tested. Treat any problems you find.
Review your meds. Talk to your doctor about all medications. Ask about memory-friendly alternatives.
Limit alcohol. If you drink, keep it moderate. No more than 14 units per week.
Get sleep apnea treated. If you snore loudly or wake up tired, get tested.
Treat depression. Don’t suffer in silence. Mental health care protects brain health.
Stay curious. Learn new things. Challenge your brain with puzzles, reading, or new skills.
Conclusion
Memory loss at any age deserves attention.
Yes, some forgetting is normal. But you shouldn’t accept it without question. Many causes are treatable. Caught early, you can often reverse the damage or stop it from getting worse.
Don’t Google your symptoms and assume the worst. But don’t ignore them either.
If memory problems worry you, talk to a neurologist. They can run tests to find the cause. They can create a treatment plan that addresses your specific situation.
Your brain is amazing. It’s capable of change and growth at any age. Give it the support it needs.
Start with one change today. Better sleep. A walk. A phone call to a friend. Small steps add up to big improvements.


