The Lancet Commission on Dementia found something remarkable: up to 40% of dementia cases could be prevented or delayed through lifestyle changes. This isn’t about luck or genetics alone. It’s about daily choices that shape your brain’s future.
Understanding Dementia
Before we explore prevention strategies, let’s clarify what dementia actually is—and isn’t.
Dementia is an umbrella term for a decline in mental ability severe enough to interfere with daily life. It’s not a single disease but rather a group of symptoms affecting memory, thinking, and social abilities.
Think of dementia as the symptom (like “fever”) and the specific diseases as the causes (like “flu” or “infection”). Understanding the different types helps you grasp why prevention strategies work.
The Main Types of Dementia
Alzheimer’s Disease (60-80% of cases)
Alzheimer’s is the most common cause of dementia. It involves the buildup of two toxic proteins in the brain: amyloid-beta plaques and tau tangles. These proteins damage and kill brain cells, starting in the hippocampus (your memory center) and spreading outward.
The disease progresses slowly. Early symptoms include difficulty remembering recent events and conversations. Later stages affect language, decision-making, and eventually basic functions.
Vascular Dementia (10-20% of cases)
This type results from reduced blood flow to the brain, often after strokes or due to damaged blood vessels. When parts of your brain don’t get enough oxygen and nutrients, cells die.
Symptoms can appear suddenly after a stroke or develop gradually with small vessel disease. This type often affects planning, judgment, and processing speed before memory problems emerge.
Lewy Body Dementia (5-10% of cases)
Caused by abnormal protein deposits (Lewy bodies) throughout the brain. This type shares features with both Alzheimer’s and Parkinson’s disease.
People with Lewy body dementia often experience visual hallucinations, movement problems similar to Parkinson’s, and dramatic fluctuations in alertness and attention.
Frontotemporal Dementia (5-10% of cases)
This involves damage to the frontal and temporal lobes of the brain. It typically starts earlier than Alzheimer’s—often in the 50s and 60s.
Early symptoms include personality changes, loss of empathy, inappropriate behavior, and language problems rather than memory loss.
Mixed Dementia
Many people, particularly those over 80, have more than one type of dementia simultaneously. The most common combination is Alzheimer’s disease with vascular dementia.
Why Prevention Matters for All Types
Here’s the encouraging news: the lifestyle habits we’ll discuss protect against multiple types of dementia.
- Blood pressure control primarily prevents vascular dementia but also reduces Alzheimer’s risk
- Exercise fights both vascular damage and toxic protein buildup
- Healthy diet reduces inflammation that contributes to all dementia types
- Social engagement builds cognitive reserve that provides resilience against any form of brain damage
Think of your brain like a savings account. Every healthy habit makes a deposit. Over time, these deposits build what scientists call “cognitive reserve”—extra neural pathways that help your brain stay sharp even as you age.
Even if some brain damage occurs, cognitive reserve helps you maintain function longer. This is why two people with similar amounts of Alzheimer’s plaques in their brains can have vastly different symptoms—one person’s robust cognitive reserve lets them compensate for the damage.
What You’ll Learn in This Guide
This article covers 20 evidence-based strategies organized by impact level and life stage. You’ll discover:
- The 4 medical interventions with the strongest protective effects
- Which habits work best at different ages (early life, midlife, late life)
- Specific action steps you can implement this week
- Sample meal plans and exercise routines designed for brain health
- Quick-reference tables to track your progress
You don’t need to implement all 20 habits at once. We’ll show you how to prioritize based on your age, current health status, and risk factors.
Let’s start with the four medical safeguards that offer the strongest protection against cognitive decline.
Understanding Your Risk: The Modifiable Factors
Before we explore the habits, let’s look at which risk factors you can actually change. The Lancet Commission identified 14 modifiable risk factors across your lifespan.
| Risk Factor | Percentage of Dementia Cases | Critical Age Window | Evidence Strength |
|---|---|---|---|
| Hearing loss | 8% | Midlife (50+) | Very Strong (RCT) |
| Obesity | 8% | Midlife (40-65) | Strong |
| Education | 7% | Early life | Strong |
| Hypertension | 7% | Midlife (40-65) | Very Strong (RCT) |
| Smoking | 5% | Any age | Very Strong |
| Social isolation | 4% | Late life (65+) | Strong |
| Depression | 4% | Midlife | Moderate |
| Physical inactivity | 3% | Any age | Strong |
| Diabetes | 3% | Midlife | Strong |
| Traumatic brain injury | 3% | Any age | Strong |
| Air pollution | 2% | Any age | Moderate |
| Excessive alcohol | 1% | Any age | Strong |
Total Impact: These 12 factors account for approximately 40% of dementia cases worldwide. That means nearly half of all dementia could be prevented or delayed through lifestyle changes.
Brain Health Risk Calculator
Assess your dementia risk based on modifiable lifestyle factors
Your Risk Level
The Big 4: Medical Safeguards With Maximum Impact
These four interventions stand out for their proven ability to reduce dementia risk. Each one targets a specific biological pathway that, left unchecked, accelerates brain aging.
1. Get Your Hearing Checked—And Treated
Hearing loss tops the list of modifiable risk factors. It accounts for 8% of dementia cases worldwide.
Here’s what happens in your brain when you can’t hear properly: Your brain diverts massive resources just to process degraded sound. This leaves fewer resources for memory and thinking. Scientists call this “auditory deprivation.”
The good news? A 2024 study called the ACHIEVE trial showed hearing aids can slow cognitive decline by 48% over three years in people at increased risk.

The key is timing. Starting treatment in midlife—when hearing loss begins—provides the best protection. Waiting until severe loss develops may miss the optimal window.
Your action plan: Get an audiogram after age 50. If your audiologist recommends hearing aids, wear them consistently. Don’t wait until you “feel ready.”
Early warning signs of hearing loss:
- Asking people to repeat themselves often
- Turning up TV or radio volume higher than others prefer
- Difficulty following conversations in noisy environments
- Ringing in the ears (tinnitus)
- Feeling exhausted after social events due to listening effort
2. Control Blood Pressure in Midlife
High blood pressure damages tiny blood vessels in your brain. These micro-injuries cause white matter lesions and restrict blood flow needed to clear toxic proteins.
The critical window is midlife—ages 40 to 65. High blood pressure during these years shows the strongest link to later dementia.
The SPRINT-MIND trial found that intensive blood pressure control (keeping systolic pressure below 120) reduced mild cognitive impairment risk by 19% compared to standard targets.

One caveat: Very low blood pressure in adults over 75 may actually increase risk. Talk with your doctor about age-appropriate targets.
Your action plan: Aim for 120/80 during midlife. Check your blood pressure regularly. Work with your doctor to find the right approach—whether that’s diet, exercise, stress reduction, or medication.
Blood pressure targets by age:
- Ages 40-65: Aim for <120/80 (strongest dementia protection)
- Ages 65-75: <130/80 is often appropriate
- Ages 75+: Discuss individualized targets with your doctor (too low may increase risk)
3. Stop Smoking Now
Smoking directly poisons your neurons. It damages blood vessels, creates oxidative stress, and triggers chronic inflammation. All of this accelerates brain shrinkage and impairs the blood-brain barrier.
Current smokers face 30% to 50% higher dementia risk than people who never smoked.
But here’s the encouraging part: Quitting reverses much of this risk. Former smokers who quit decades earlier have similar dementia risk to people who never smoked at all.
Risk starts declining within five years of quitting. After 10 to 15 years, your risk approaches baseline.
Your action plan: If you smoke, quitting is the single most powerful step you can take. Talk to your doctor about cessation programs. Nicotine replacement, medications, and counseling all improve success rates.
4. Maintain a Healthy Weight in Midlife
Obesity in midlife increases dementia risk by 30% to 40%. It accounts for 8% of dementia cases.
Excess weight—particularly abdominal fat—produces inflammatory proteins that cross into your brain. These proteins interfere with how your brain processes toxic proteins like amyloid.
The relationship gets more complex after age 65. Low weight in late life may signal underlying disease rather than protection.
Focus on metabolic health, not just the number on the scale. People who are metabolically healthy at higher weights may have lower risk than metabolically unhealthy people at “normal” weights.
Your action plan: Pay attention to your weight between ages 40 and 60. Focus on waist-to-hip ratio. Build sustainable habits around nutrition and movement rather than crash diets.
Metabolic health markers to track:
- Waist circumference (men <40 inches, women <35 inches)
- Waist-to-hip ratio (men <0.9, women <0.85)
- Fasting glucose (<100 mg/dL)
- HbA1c (<5.7%)
- Blood pressure (<120/80)
- Triglycerides (<150 mg/dL)
Move Your Body, Build Your Brain
Physical activity protects your brain through multiple pathways. Different types of exercise offer distinct benefits.
| Day | Activity Type | Duration | Primary Brain Benefit |
|---|---|---|---|
| Monday | Brisk walking or cycling | 30 minutes | Memory (BDNF production) |
| Tuesday | Strength training | 30-40 minutes | Executive function |
| Wednesday | Swimming or dancing | 30 minutes | Memory + coordination |
| Thursday | Strength training | 30-40 minutes | Executive function |
| Friday | Yoga or tai chi | 30 minutes | Balance + stress reduction |
| Saturday | Hiking or sports | 45-60 minutes | Memory + social engagement |
| Sunday | Active rest (gentle walking) | 20-30 minutes | Recovery + movement breaks |
Total weekly target: 150 minutes moderate cardio + 2-3 strength sessions
5. Do Aerobic Exercise for Memory
Cardio triggers release of Brain-Derived Neurotrophic Factor, or BDNF. Think of BDNF as fertilizer for your hippocampus—the brain region that forms new memories.
A landmark 2011 study showed one year of aerobic exercise (40 minutes, three times per week) increased hippocampal volume by 2% in older adults. This essentially reversed one to two years of age-related shrinkage.
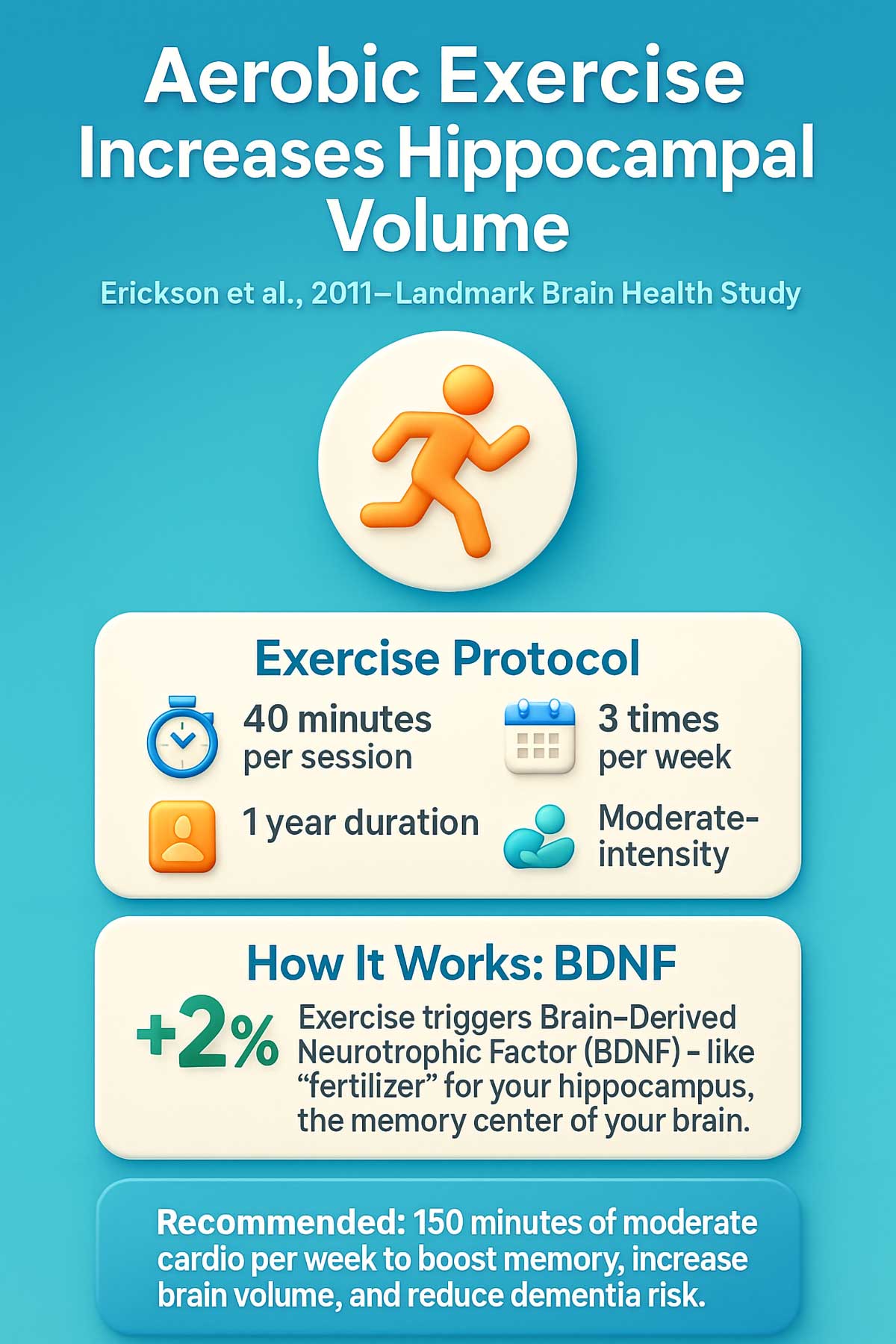
Aerobic exercise also improves blood flow, reduces inflammation, and enhances how neurons communicate with each other.
Your action plan: Aim for 150 minutes of moderate cardio per week. That’s about 30 minutes, five days a week. Brisk walking, swimming, cycling, or dancing all count. Pick activities you enjoy enough to sustain long-term.
How to know you’re at “moderate intensity”:
- You can talk but not sing during the activity
- Heart rate is 50-70% of maximum (220 minus your age)
- You feel slightly breathless but not gasping
- You could maintain the pace for 30-60 minutes
Best aerobic exercises for brain health:
- Brisk walking (easiest to sustain long-term)
- Swimming (low impact, full body)
- Cycling (outdoor or stationary)
- Dancing (adds coordination and social elements)
- Water aerobics (joint-friendly option)
6. Lift Weights for Executive Function
Strength training releases different brain-protective compounds than cardio does. Muscles produce hormones called myokines that cross into your brain and specifically benefit your frontal lobe.
Your frontal lobe handles executive functions—planning, decision-making, multitasking. These are the cognitive abilities you need for daily independence.
Research shows resistance training two to three times per week improves attention and slows white matter lesion progression.
Your action plan: Strength train two to three days per week. Target major muscle groups. Start with bodyweight exercises or light weights. Gradually increase resistance as you get stronger.
Simple strength training routine for beginners (2-3 sets of 10-12 reps):
- Squats or chair sits (legs)
- Push-ups or wall push-ups (chest, arms)
- Rows with resistance band (back)
- Shoulder press with light weights (shoulders)
- Planks (core, hold 20-30 seconds)
- Bicep curls (arms)
Progression tips: Start with bodyweight only. Add resistance when exercises feel easy. Rest 48 hours between sessions for the same muscle groups.
7. Break Up Sitting Time
Sitting for eight or more hours daily is linked to thinner brain regions, even in people who exercise regularly.
Prolonged sitting appears to have effects beyond simply not exercising. It may impair glucose metabolism, increase inflammation, and reduce blood flow to your brain.
A 2018 study found that sedentary time associated with a thinner medial temporal lobe—your brain’s memory center—independent of physical activity levels.
Your action plan: Set a timer for every 30 minutes. Stand up and move for at least two minutes. Walk to get water. Do some stretches. Take a lap around your office. These “exercise snacks” may offset some risks of sitting.
8. Focus on Metabolic Health
We covered weight in the Big 4, but metabolic health deserves its own mention.
Type 2 diabetes increases Alzheimer’s risk by about 50% and vascular dementia risk by 100%. Even prediabetes and insulin resistance raise your risk.
Diabetes creates multiple problems: vascular damage, chronic inflammation, insulin resistance in the brain, and impaired clearance of toxic proteins.
Preventing diabetes through lifestyle appears more protective than aggressive treatment after diagnosis.
Your action plan: Monitor your HbA1c levels annually if you’re at risk. Focus on prevention through the habits in this article: exercise, healthy eating, adequate sleep, stress management.
Eat to Protect Your Brain
Nutrition matters for brain health. Certain dietary patterns show consistent protective effects.
| Food Category | MIND Diet Target | Brain Benefits | Examples |
|---|---|---|---|
| Leafy greens | 6+ servings/week | Vitamin K, folate, antioxidants | Spinach, kale, collards, arugula |
| Other vegetables | 1+ serving/day | Fiber, antioxidants | Broccoli, peppers, carrots, beets |
| Berries | 2+ servings/week | Flavonoids reduce inflammation | Blueberries, strawberries, blackberries |
| Nuts | 5+ servings/week | Vitamin E, healthy fats | Walnuts (best), almonds, pistachios |
| Whole grains | 3+ servings/day | Fiber, B vitamins | Oats, brown rice, whole wheat, quinoa |
| Fish | 1+ serving/week | Omega-3 fatty acids | Salmon, mackerel, sardines, trout |
| Beans | 3+ servings/week | Protein, fiber, minerals | Lentils, chickpeas, black beans |
| Poultry | 2+ servings/week | Lean protein | Chicken, turkey |
| Olive oil | Primary cooking fat | Anti-inflammatory | Extra virgin olive oil |
| Wine (optional) | ≤1 glass/day | Limit or avoid for brain health | Red wine if any |
Foods to limit:
- Red meat: <4 servings/week
- Butter and margarine: <1 tablespoon/day
- Cheese: <1 serving/week
- Pastries and sweets: <5 servings/week
- Fried or fast food: <1 serving/week
9. Follow the MIND Diet Principles
The MIND diet combines Mediterranean and DASH diets with specific emphasis on brain-protective foods.
High adherence to the MIND diet associates with 35% to 53% lower Alzheimer’s risk in observational studies.
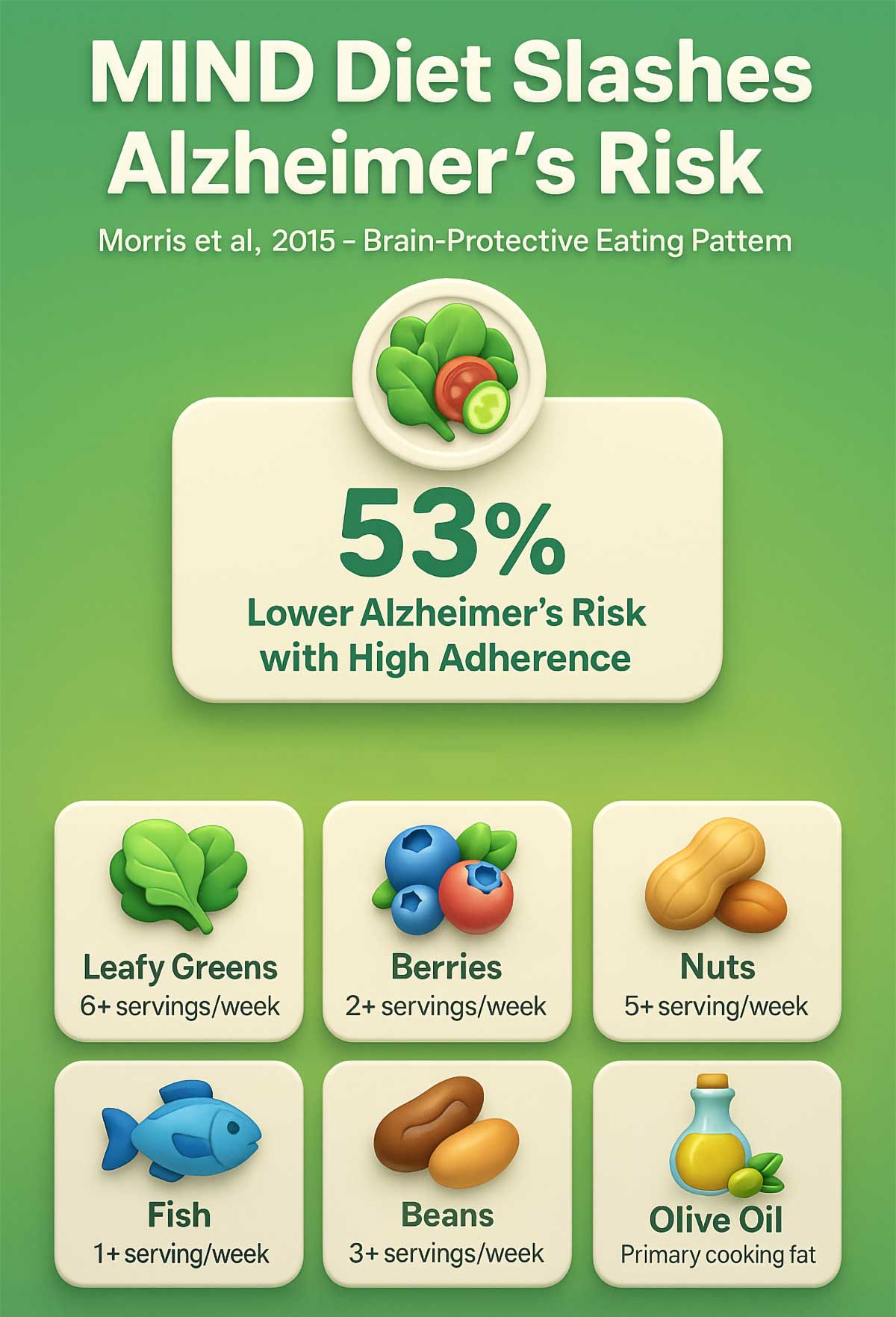
The diet emphasizes leafy greens, berries, nuts, whole grains, fish, and olive oil. It limits red meat, butter, cheese, pastries, and fried foods.
Why these foods? They provide anti-inflammatory compounds, antioxidants, and nutrients that support vascular health and reduce oxidative stress.
Your action plan: Use the “greens and berries” rule. Eat leafy greens daily. Have berries at least twice per week. Add nuts, fish, and olive oil regularly. Cut back on processed foods, red meat, and fried items.
Sample 3-Day MIND Diet Meal Plan
Day 1
- Breakfast: Oatmeal with blueberries, walnuts, and cinnamon
- Lunch: Large spinach salad with grilled chicken, chickpeas, olive oil dressing
- Snack: Apple slices with almond butter
- Dinner: Baked salmon with roasted broccoli and quinoa
- Hydration: Water, green tea
Day 2
- Breakfast: Whole grain toast with avocado and scrambled eggs
- Lunch: Lentil soup with kale and whole grain bread
- Snack: Mixed berries with a handful of walnuts
- Dinner: Turkey and vegetable stir-fry with brown rice
- Hydration: Water, herbal tea
Day 3
- Breakfast: Greek yogurt with strawberries and ground flaxseed
- Lunch: Quinoa bowl with black beans, peppers, greens, olive oil
- Snack: Carrot sticks with hummus
- Dinner: Grilled chicken with sweet potato and Brussels sprouts
- Hydration: Water, chamomile tea
Brain-Boosting Snack Ideas:
- Trail mix (walnuts, almonds, dried blueberries—unsweetened)
- Apple or pear with nut butter
- Hummus with vegetable sticks
- Plain Greek yogurt with berries
- Dark chocolate (70%+ cacao) with almonds (small portions)
10. Rethink Alcohol Consumption
The science on alcohol and brain health has shifted dramatically.
Older research suggested moderate drinking might protect the brain. Newer evidence challenges this view.
Alcohol is a neurotoxin. It shrinks the hippocampus, disrupts sleep architecture needed for memory consolidation, and interferes with your brain’s waste removal system.
Heavy drinking (more than 21 units per week) clearly increases dementia risk by 20% to 40%. But recent genetic studies suggest there may be no safe level for brain health.
Your action plan: If you drink, less is better. The safest choice for brain health is minimal or no alcohol. If you choose to drink, keep it truly moderate—and know it’s not providing brain benefits.
Understanding alcohol units:
- 1 standard drink = 5 oz wine, 12 oz beer, or 1.5 oz spirits
- Heavy drinking = >14 drinks/week for men, >7 for women
- Moderate drinking = 1 drink/day for women, 2 for men
- Brain-optimal = Minimal or none
Why the science changed: Older studies showing benefits often compared drinkers to abstainers who quit due to health problems. When accounting for this, the protective effect disappeared.
11. Add Anti-Inflammatory Foods
Chronic inflammation “fogs” neural signaling. It interferes with how brain cells communicate.
Omega-3 fatty acids, found in fatty fish and walnuts, help reduce inflammation. Dark-skinned fruits provide antioxidants that fight oxidative stress.
These foods support vascular health and may slow cognitive aging.
Your action plan: Eat fatty fish like salmon, mackerel, or sardines twice per week. Snack on walnuts. Include colorful berries and other fruits regularly. These foods work best as part of an overall healthy pattern.
| Food | Key Compound | How Much | Brain Benefit |
|---|---|---|---|
| Fatty fish | Omega-3 (DHA/EPA) | 2 servings/week | Reduces inflammation, builds cell membranes |
| Walnuts | ALA omega-3, vitamin E | 1 oz (7 walnuts)/day | Fights oxidative stress |
| Blueberries | Anthocyanins | ½ cup, 2-3x/week | Crosses blood-brain barrier, reduces oxidation |
| Strawberries | Flavonoids | 1 cup, 2x/week | Improves neural communication |
| Dark leafy greens | Vitamin K, lutein | 1 cup/day | Slows cognitive aging |
| Turmeric | Curcumin | ½ tsp/day in food | Anti-inflammatory (add black pepper for absorption) |
| Extra virgin olive oil | Oleocanthal | 2-3 Tbsp/day | Reduces brain inflammation |
Simple anti-inflammatory smoothie recipe:
- 1 cup spinach
- ½ cup blueberries
- ½ banana
- 1 Tbsp ground flaxseed
- 1 Tbsp walnuts
- 1 cup unsweetened almond milk
- ½ tsp turmeric
- Pinch of black pepper
Blend until smooth. Provides omega-3s, antioxidants, and anti-inflammatory compounds in one glass.
12. Check Your B12 and Homocysteine Levels
High homocysteine levels are toxic to neurons and accelerate brain shrinkage. B vitamins (B12, B6, folate) help break down homocysteine into harmless compounds.
The VITACOG trial showed B-vitamin supplements slowed brain atrophy by 30%—but only in people with elevated homocysteine. No benefits occurred in those with normal levels.
This is targeted intervention for deficiency, not universal supplementation.
Who’s at risk? Older adults, vegans and vegetarians, people taking metformin or proton pump inhibitors, and those with certain genetic variants.
Your action plan: Test your B12 and homocysteine levels, especially if you’re over 60 or follow a plant-based diet. Supplement only if levels are low. Work with your doctor to determine appropriate doses.
When to test B12 and homocysteine:
- Age 60+ (annual screening recommended)
- Following vegan or vegetarian diet
- Taking metformin for diabetes
- Taking proton pump inhibitors (PPIs) for acid reflux
- History of digestive disorders
- Unexplained fatigue or memory issues
Optimal levels:
- Vitamin B12: >400 pg/mL (some experts recommend >500)
- Homocysteine: <10 μmol/L (lower is better)
- Folate: >10 ng/mL
Food sources of B vitamins:
- B12: Fish, meat, eggs, fortified cereals (no plant sources)
- Folate: Leafy greens, beans, lentils, fortified grains
- B6: Chickpeas, salmon, chicken, potatoes
Build Cognitive and Emotional Armor
Your brain needs more than just physical health. Cognitive engagement, emotional wellbeing, and quality sleep all build resilience.
13. Prioritize Deep Sleep
During deep sleep, your brain’s waste removal system—the glymphatic system—becomes highly active. It physically flushes out toxic proteins like amyloid-beta and tau.
Sleep also consolidates memories and allows cellular repair.
Both short sleep (less than six hours) and long sleep (more than nine hours) associate with increased dementia risk. The optimal range appears to be seven to eight hours with good quality.
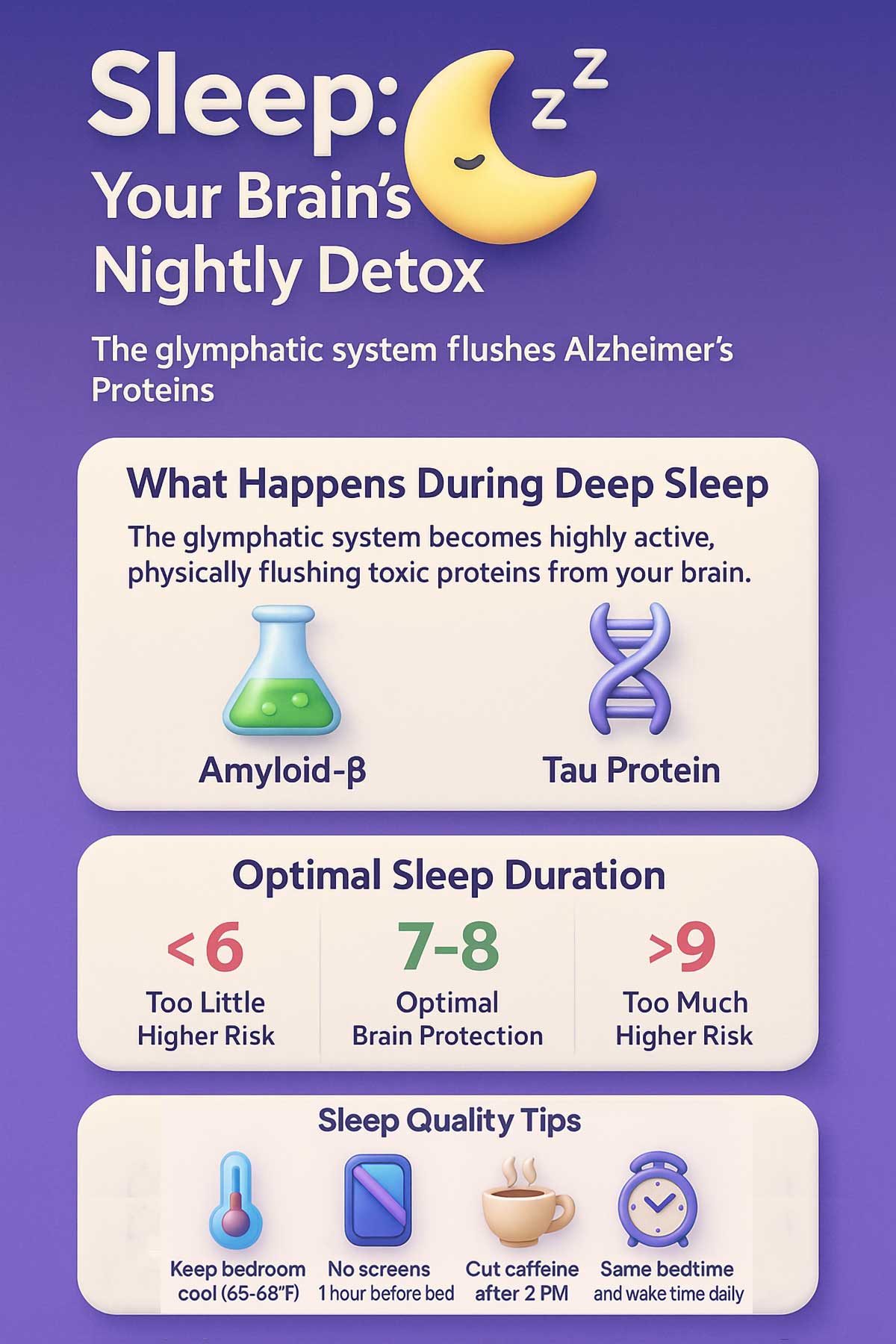
Sleep disorders matter too. Obstructive sleep apnea prevents the deep sleep stages needed for waste clearance. Treating sleep apnea with CPAP may slow cognitive decline.
Your action plan: Aim for seven to eight hours of consolidated sleep. If you snore loudly or feel tired despite adequate sleep time, ask your doctor about sleep apnea testing. Treat diagnosed sleep disorders aggressively.
Warning signs of sleep apnea:
- Loud, persistent snoring
- Gasping or choking during sleep
- Morning headaches
- Excessive daytime sleepiness
- Difficulty concentrating
- Witnessed breathing pauses during sleep
Sleep apnea affects 30% of adults over 65 and dramatically reduces deep sleep quality. Treatment can improve cognitive outcomes.
14. Learn Genuinely New Skills
Passive activities like watching TV don’t build cognitive reserve. You need active learning that’s difficult enough to be frustrating at first.
Learning new complex skills—languages, musical instruments, challenging hobbies—creates new neural pathways. These extra pathways help your brain function even if damage occurs.
The key word is “new.” Doing crossword puzzles you’ve mastered doesn’t provide the same benefit as tackling genuinely unfamiliar challenges.
Your action plan: Pick a complex skill you’ve always wanted to learn. Language learning apps, music lessons, or dance classes all work. Stick with it long enough to move past the frustrating beginner phase. The struggle itself builds cognitive reserve.
| Activity | Cognitive Domains Engaged | Time Commitment | Getting Started |
|---|---|---|---|
| Learning a language | Memory, attention, multitasking | 30 min/day | Apps like Duolingo, community classes |
| Musical instrument | Fine motor, memory, coordination | 20-30 min/day | Rent before buying, online tutorials |
| Dancing | Coordination, memory, social | 1-2 hours/week | Community dance classes, YouTube tutorials |
| Complex games | Strategy, planning, problem-solving | Variable | Chess, bridge, strategic board games |
| Creative writing | Language, imagination, planning | 20-30 min/day | Writing groups, online courses |
| Painting or drawing | Visual-spatial, fine motor | 1-2 hours/week | Community art classes, online tutorials |
Why difficulty matters: Easy activities don’t build new neural pathways. The brain adapts to challenges. If you’re not occasionally frustrated, you’re not learning at the optimal level.
The 70% rule: Choose activities where you succeed about 70% of the time. This balance keeps you challenged without becoming discouraged.
15. Find Purpose and Meaning
People with a strong sense of purpose show less cognitive decline even when they have Alzheimer’s pathology in their brains.
A 2010 study found that people with high “purpose in life” scores maintained better cognitive function even when autopsy showed significant brain damage.
Purpose may work through multiple pathways: reducing stress hormones, promoting healthy behaviors, increasing cognitive engagement, and strengthening social connections.
Your action plan: Get involved in activities that feel meaningful. Volunteer. Mentor someone. Take on community roles. The specific activity matters less than the sense of contribution it provides.
16. Stay Socially Connected
Social isolation damages your brain as much as smoking does. It accounts for 4% of dementia cases.
Social interaction is the most complex cognitive task humans perform. It exercises multiple brain regions simultaneously while reducing stress and promoting physical activity.
A 12-year study showed that larger social networks predicted slower cognitive decline, independent of baseline cognitive ability.
Quality matters more than quantity. Meaningful relationships provide greater protection than superficial contacts.
Your action plan: Prioritize face-to-face interactions. Join clubs or groups around your interests. Attend community events. If you’re isolated, start small—one meaningful connection is better than none.
Combating social isolation—practical steps:
If you’re working:
- Eat lunch with coworkers instead of at your desk
- Join workplace committees or social groups
- Attend industry networking events
If you’re retired:
- Volunteer for causes you care about (libraries, schools, hospitals)
- Take classes at community colleges or senior centers
- Join hobby groups (book clubs, gardening, crafts)
- Participate in religious or spiritual communities
For everyone:
- Schedule regular phone or video calls with distant friends/family
- Invite someone for a walk instead of just texting
- Say yes to social invitations even when you’d rather stay home
- Consider getting a dog (provides companionship and social opportunities during walks)
Quality over quantity: Two meaningful friendships protect your brain more than ten superficial acquaintances. Look for relationships where you can be authentic and feel supported.
17. Treat Depression as a Medical Priority
Depression doubles dementia risk. It accounts for 4% of dementia cases.
Depression elevates cortisol, which is toxic to the hippocampus. It also reduces BDNF, increases inflammation, and may accelerate brain shrinkage.
Timing matters. Midlife depression shows a stronger link to later dementia than late-life depression. This suggests depression may cause brain changes rather than simply being an early symptom.
Your action plan: Don’t dismiss persistent low mood as “just stress.” Talk to your doctor. Depression is a medical condition that deserves treatment for both your current wellbeing and long-term brain health.
18. Manage Chronic Stress
Chronic stress shrinks your prefrontal cortex—the brain region handling complex thinking and decision-making.
Stress elevates cortisol continuously. High cortisol directly damages the hippocampus, accelerates cellular aging, and promotes inflammation. Stress also disrupts sleep and encourages unhealthy coping behaviors.
Mindfulness meditation and other stress reduction techniques show benefits for cognitive complaints and may support overall brain health.
Your action plan: Find stress management approaches that work for you. Meditation, yoga, time in nature, social support, and therapy all help. The goal isn’t to eliminate stress entirely—that’s impossible. It’s to prevent chronic, unmanaged stress from wearing down your brain.
Simple stress reduction techniques to try:
5-minute practices (do daily):
- Deep breathing: Breathe in for 4 counts, hold for 4, out for 6. Repeat 5 times.
- Progressive muscle relaxation: Tense and release each muscle group
- Gratitude journaling: Write 3 things you’re grateful for
20-minute practices (3-5 times weekly):
- Mindfulness meditation: Focus on breath, notice thoughts without judgment
- Gentle yoga or stretching
- Nature walk without phone
- Listen to calming music
Weekly practices:
- Spend time with supportive friends or family
- Engage in a hobby you enjoy
- Get a massage or other relaxing self-care
- Attend religious or spiritual services if that resonates
Signs your stress needs professional help:
- Physical symptoms (headaches, digestive issues, muscle tension)
- Sleep problems lasting more than 2 weeks
- Difficulty concentrating or making decisions
- Feeling overwhelmed most days
- Using alcohol or food to cope
A therapist can teach evidence-based techniques like cognitive behavioral therapy (CBT) that reduce stress hormones and protect your brain.
19. Choose Real Learning Over Brain Games
Commercial brain training apps often promise more than they deliver.
The ACTIVE trial showed that cognitive training improved specific trained abilities for up to 10 years. But benefits rarely transferred to untrained tasks or daily functioning.
Learning genuinely new skills provides broader cognitive engagement. It integrates multiple cognitive systems in ways that simple computer games don’t.
Your action plan: Skip the brain training subscriptions. Invest that time and money in learning real skills instead. Take a class. Learn an instrument. Study a language. These activities provide deeper, more meaningful cognitive challenges.
Protect Your Brain From Environmental Factors
Some risk factors come from your environment rather than your choices. You can’t control everything, but you can reduce exposure.
20. Reduce Air Pollution Exposure
Fine particulate matter (PM2.5) crosses the blood-brain barrier. It promotes inflammation and may accelerate toxic protein buildup.
Air pollution accounts for about 2% of dementia cases. Traffic-related pollution shows particularly strong associations.
Individual control is limited. This is primarily a public health issue requiring policy changes. But you can take some steps to reduce exposure.
Your action plan: Check air quality indexes before outdoor exercise. Avoid high-traffic areas during peak pollution hours. Use HEPA filters in your home, especially in bedrooms. Support clean air policies in your community.
Bonus: The Missing Risk Factor
Physical brain trauma triggers chronic inflammation and accelerates toxic protein accumulation. Even mild concussions increase later dementia risk. The effects are cumulative across multiple injuries.
Your action plan: Wear helmets during cycling, motorcycling, and contact sports. Use seatbelts consistently. Take fall prevention seriously as you age. Avoid unnecessary high-risk activities.
Putting It All Together: Your Brain Protection Plan
Twenty habits can feel overwhelming. Don’t try to change everything at once.
Your Personalized Starting Point by Age
If You’re in Your 40s-50s (Midlife Prevention)
Top 5 priorities:
- Get blood pressure under control (<120/80)
- Maintain healthy weight and metabolic health
- Establish exercise routine (150 min cardio + strength training)
- Get baseline hearing test
- Quit smoking if applicable
Why now matters: Midlife is the critical window for preventing vascular damage. What you do now determines your brain health 20-30 years from now.
If You’re in Your 60s-70s (Late-Life Protection)
Top 5 priorities:
- Treat hearing loss aggressively (biggest single intervention)
- Stay physically active (prevent sedentary decline)
- Maintain social connections (join groups, volunteer)
- Get quality sleep (treat sleep apnea if present)
- Keep learning new skills (languages, instruments, hobbies)
Why now matters: You can still build cognitive reserve. The brain maintains plasticity throughout life.
If You’re in Your 80s+ (Maximizing Function)
Top 5 priorities:
- Stay socially engaged (quality relationships)
- Move daily (walking, gentle exercise)
- Continue mentally stimulating activities
- Optimize nutrition (Mediterranean/MIND diet)
- Manage chronic conditions (diabetes, BP, hearing)
Why now matters: Cognitive reserve built earlier in life pays dividends now. Continued engagement maintains function.
30-Day Brain Health Starter Plan
Can’t do everything at once? This progressive plan helps you build habits gradually.
Week 1: Assess and Baseline
- Day 1-2: Track current habits (sleep, exercise, diet)
- Day 3-4: Schedule medical appointments (hearing test, BP check, labs)
- Day 5-7: Choose one habit to start (pick your biggest gap)
Week 2: Movement Foundation
- Add 20-30 minutes of walking daily
- Try one new physical activity
- Set up standing/movement reminders if you sit a lot
Week 3: Nutrition Upgrades
- Add leafy greens to one meal daily
- Replace one snack with nuts or berries
- Cook one brain-healthy recipe from this guide
Week 4: Cognitive and Social
- Sign up for one new learning activity or class
- Schedule social time with at least 2 people
- Begin a simple stress reduction practice (5-min breathing)
By Day 30, you’ll have:
- Medical baseline data
- Daily movement habit
- Improved nutrition
- Started cognitive/social engagement
- Basic stress management routine
Conclusion
Start with these three actions this week:
- Schedule appointments: Get your hearing tested, blood pressure checked, and baseline labs drawn (glucose, B12, homocysteine).
- Choose your first habit: Pick one area where you have the biggest gap. If you’re sedentary, start walking. If you eat poorly, add greens daily. If you’re isolated, join one group.
- Track your progress: Use the habit tracker above. Seeing your consistency builds motivation.
Remember the 40% statistic from the Lancet Commission. Nearly half of dementia cases are preventable through the habits in this guide.
Your brain is more resilient than you might think. It can build new connections throughout life. Every positive choice you make today registers in your biology tomorrow.
The 40% preventable statistic represents one of the most significant public health opportunities of our time. You have more control over your cognitive future than previous generations believed possible.
There’s no magic pill for preventing dementia. But there is a magic combination: sustained healthy habits across multiple domains, started as early as possible and maintained throughout life.
FAQs
Is it ever too late to start?
No. The brain maintains plasticity throughout life. Starting protective habits at any age provides benefits. The earlier you start, the more protection you build, but late action is better than no action.
Can I reverse existing cognitive decline?
Mild cognitive impairment sometimes improves with intensive lifestyle intervention. Established dementia can’t be reversed, but progression may slow. Prevention is always easier than treatment.
Do I need all 20 habits to see benefits?
No. Even implementing 3-5 key habits significantly reduces risk. Start with the Big 4 medical factors, then add habits that fit your lifestyle.
How long before I see results?
Some benefits (mood, sleep quality, energy) appear within weeks. Structural brain changes (increased hippocampal volume from exercise) take 6-12 months. Dementia risk reduction accumulates over years to decades.
What about supplements and “brain boosting” pills?
For most people with adequate nutrition, supplements don’t help. The exception is B12 supplementation if you’re deficient. Get nutrients from whole foods first. Test before supplementing.
Does family history mean I’m destined to get dementia?
No. Genetics account for less than 10% of late-onset Alzheimer’s cases. Even people with the APOE4 gene variant can significantly reduce risk through lifestyle factors.
Which single habit has the biggest impact?
There’s no single “magic habit.” The combination matters most. If forced to choose one, regular aerobic exercise has the broadest benefits—it helps with weight, blood pressure, mood, sleep, and directly triggers BDNF production.


